Syncope
Content is incomplete and may be incorrect. |
Definition
Syncope is a transient loss of consciousness (TLOC) due to global cerebral hypoperfusion characterized by rapid onset, short duration and spontaneous complete recovery. This excludes other causes of TLOC such as neurological, psychological and metabolic causes.
Classification
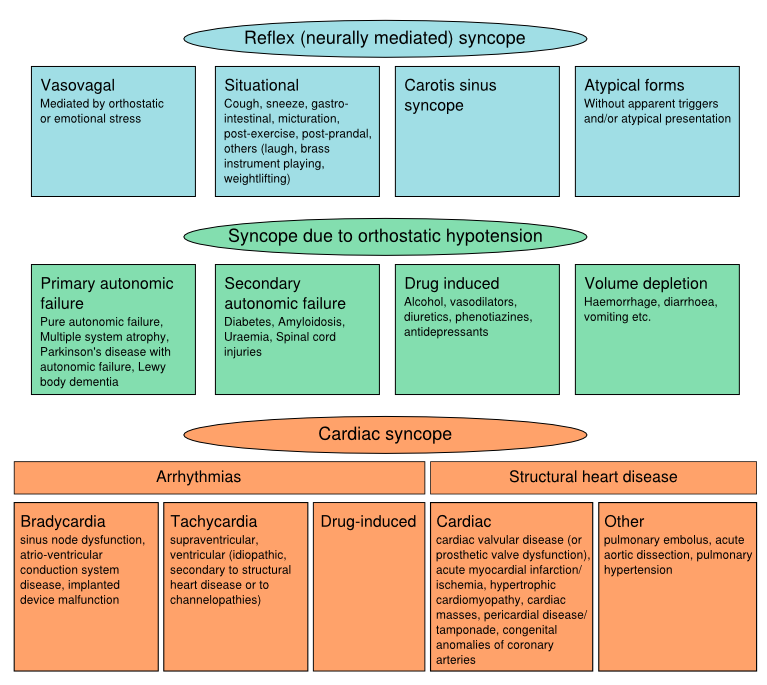
Syncope can be classified into:
Pathophysiology
(Figure pathophysiology syncope)
Epidemiology
Syncope is common in the general population. The life-time cumulative incidence of ≥1 syncopal episodes in teenagers in the general population is high, with about 40 % by the age of 21 years. Reflex syncope is by far the most common cause. The majority have experienced reflex-mediated syncope episodes as teenagers and adolescents. The frequency of orhtostatic hypotension and cardiac syncope increases with age. Approximately 10-30% of the syncope episodes in patients above 60 years visiting a hospital for their syncope episodes are of cardiac origin.
Clinical features
History taking is the most important feature in syncope evaluation. These clinical features suggestive of a specific cause of syncope:
| Reflex (neurally mediated) syncope |
|---|
| Absence of cardiac disease |
| Long history of syncope |
| After sudden, unexpected, unpleasant sight, sound, smell, or pain |
| Prolonged standing or crowded, hot places |
| Nausea, vomiting associated with syncope |
| During or in the absorptive state after a meal |
| With head rotation, pressure on carotid sinus (as in tumous, shaving, tight collars) |
| After exertion |
| Syncope due to orthostatic hypotension |
| After standing up |
| Temporal relationship with start of medication leading to hypotension or changes of dosage |
| Prolonged standing especially in crowded, hot places |
| Presence of autonomic neuropathy or Parkinsonism |
| After exertion |
| Cardiac syncope |
| Presence of severe structural heart disease |
| During exertion, or supine |
| Preceded by palpitation or accompanied by chest pain |
| Family history of sudden death |
In all patients presenting to a physician with syncope an ECG is recommended to screen for a cardiac cause of syncope. Holter monitoring is indicated only in patients who have very frequent syncopes or presyncope. In-hospital monitoring (in bed or telemetric) is warranted only when the patient has important structural heart disease and is at high risk of life-threatening arrhythmias.
When the mechanism of syncope remains unclear after full evaluation, an implantable loop recorder is indicated in patients who have clinical or ECG features suggesting arrhythmic syncope.
Reflex syncope
Diagnostic evaluation
Reflex syncope refers to a heterogeneous group of conditions in which there is a relatively sudden change in autonomic nervous system activity (decreased sympathic tonus causing less vasoconstriction and increased parasympathic (vagal) tonus causing bradycardia), triggered by a central (e.g. emotions, pain, blood phobia) or peripheral (e.g. prolonged orthostasis or increased carotid sinus afferent activity). It leads to a fall in blood pressure and cerebral perfusion. The range of bradycardia varies widely in reflex syncope, from a small reduction in peak heart rate to several seconds of asystole. As reflex syncope requires a reversal of the normal autonomic outflow, it usually occurs in people with a functional autonomic nervous system and should therfore be distinguished from syncope due to neurogenic orthostatic hypotension in patients with chronic autonomic failure.
Adequate history taking reveals the clinical features associated with a syncopal event that are important to differentiate the different causes of syncope. Vasovagal syncope, a specific form of reflex syncope, is diagnosed if syncope is precipitated by emotional distress or orthostatic stress and is associated with typical prodrome (such as nausea, warmth, pallor, lightheadedness, and/or diaphoresis).
Treatment
The prognosis of reflex syncope is excellent. However, syncope episodes can have a considerable impact on quality of life, because of its unexpected nature and fear for recurrences. Initial treatment of reflex syncope consists of non-pharmacological treatment measures, including reassurance regarding the benign nature of the condition, increasing the dietary salt and fluid intake, moderate exercise training, and physical counterpressure maneuvres (muscle tensing).
Orthostatic hypotension
Diagnostic evaluation
Orthostatic hypotension is a sustained reduction of systolic blood pressure of at least 20 mmHg or diastolic blood pressure of 10 mmHg within 3 min of standing or head-up tilt to at least 60 degree on a tilt table. Orthostatic hypotension is a clinical sign and may be symptomatic or asymptomatic.