Cardiac Arrest: Difference between revisions
| (17 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
''Sébastien Krul, MD, Jonas de Jong, MD'' | ''Sébastien Krul, MD, Jonas de Jong, MD'' | ||
=Introduction= | =Introduction= | ||
Survival of cardiac arrest continues to be very poor. In-hospital cardiac arrest has a survival to hospital discharge of 17,6% all rhythms<cite>Meaney</cite>. Out-of-hospital cardiac arrest has a worse survival with 10,7% survival to hospital discharge for all rhythms.<cite>Atwood</cite> Survival is dependent on the characteristics of the cardiac arrest (rhythm), on the patient’s medical history, and the time between the cardiac arrest en start of resuscitation.<cite>Waalewijn, Holmberg1, Holmberg2</cite> The introduction of the automated external defibrillator (AED) has dramatically increased survival of out-of-hospital cardiac arrest victims.<cite>ESC, Nolan1</cite> In this chapter we give an overview of basic life support (BLS) and advanced life support (ALS) based on the recommendation of the European Resuscitation Council Guidelines for Resuscitation 2010. | Survival of cardiac arrest continues to be very poor. In-hospital cardiac arrest has a survival to hospital discharge of 17,6% all rhythms<cite>Meaney</cite>. Out-of-hospital cardiac arrest has a worse survival with 10,7% survival to hospital discharge for all rhythms.<cite>Atwood</cite> Survival is dependent on the characteristics of the cardiac arrest (rhythm), on the patient’s medical history, and the time between the cardiac arrest en start of resuscitation.<cite>Waalewijn, Holmberg1, Holmberg2</cite> The introduction of the automated external defibrillator (AED) has dramatically increased survival of out-of-hospital cardiac arrest victims.<cite>ESC, Nolan1</cite> In this chapter we give an overview of basic life support (BLS) and advanced life support (ALS) based on the recommendation of the European Resuscitation Council Guidelines for Resuscitation 2010. | ||
| Line 15: | Line 14: | ||
====Foreign body airway obstruction==== | ====Foreign body airway obstruction==== | ||
An obstruction of the airway is uncommon, but reversible and adequate recognition can prevent cardiac arrest.<cite>Fingerhut</cite> Airway obstruction is usually related | An obstruction of the airway is uncommon, but reversible and adequate recognition can prevent cardiac arrest.<cite>Fingerhut</cite> Airway obstruction is usually related to eating. In a mild obstruction patients can cough and speak and only frequent reassessment is advised. Patients that have a severe obstruction are unable to speak and have problems breathing and coughing. If a patient is still conscious five back blows can be applied between the shoulder blades whilst the patient leans forward. Otherwise five abdominal thrusts can be applied by clenching a fist and grasping it with the other hand. Place the hands it between the rib-cage and the umbilicus and pull sharply inward and upward whilst standing behind the patients.<cite>Guildner, Ruben</cite> If the patient loses consciousness start BLS.<cite>Koster2</cite> | ||
====Basic life support in children==== | ====Basic life support in children==== | ||
| Line 26: | Line 25: | ||
==Preventing in Hosptial Cardiac Arrest== | ==Preventing in Hosptial Cardiac Arrest== | ||
[[File:MEWS.svg|thumb|500px|right|'''Figure 2.''' An example of a MEWS<cite>IHI</cite>.]] | [[File:MEWS.svg|thumb|500px|right|'''Figure 2.''' An example of a MEWS. Adapted from: <cite>IHI</cite>.]] | ||
The best way to prevent sudden death is to early detect deterioration of a patient and to act on early warning signs.<cite>Smith</cite> An early warning score (Figure 2) helps to create consensus among care providers about the sickness of a patient.<cite>Hodgetts, Hillman</cite> If the summed score | The best way to prevent sudden death is to early detect deterioration of a patient and to act on early warning signs.<cite>Smith</cite> Cardiac arrest is rarely unpredictable and is precipitated by a slow deterioration. An early warning score (Figure 2) helps to create consensus among care providers about the sickness of a patient.<cite>Hodgetts, Hillman</cite> If the summed score reached a certain threshold, a doctor should be notified. The notified doctor should assess the patient within 30 minutes and discuss a treatment plan. If the patient does not improve within 60 minutes a reassessment should follow with possible inclusion of a medical emergency team (MET) or intensive care specialist.<cite>Bellomo</cite> | ||
==Advanced Life Support (ALS)== | ==Advanced Life Support (ALS)== | ||
| Line 36: | Line 35: | ||
====Patient assessment==== | ====Patient assessment==== | ||
During a cardiac arrest a structured assessment of the patient is required to detect the effects of the resuscitation, return of spontaneous circulation, reversible causes. To facilitate this assessment, an ABCDE approach can be used.<br> | During a cardiac arrest a structured assessment of the patient is required to detect the effects of the resuscitation, return of spontaneous circulation, reversible causes. To facilitate this assessment, an ABCDE approach can be used.<cite>Thim, Guly</cite><br> | ||
'''Airway:''' During the first step it is important to assess if the airway is clear. Airway obstruction can occur at any level. It can be caused by obstruction from the soft palate and epiglottis, blood, vomit and foreign bodies or airway oedema. It is important to look, listen and feel for airway obstruction. Look for chest and abdominal movements, listen and feel for airflow at the mouth and nose. In partial airway obstruction, the inspiration or expiration is usually noisy by an inspiratory stridor or expiratory wheeze.<br> | '''Airway:''' During the first step it is important to assess if the airway is clear. Airway obstruction can occur at any level. It can be caused by obstruction from the soft palate and epiglottis, blood, vomit and foreign bodies or airway oedema. It is important to look, listen and feel for airway obstruction. Look for chest and abdominal movements, listen and feel for airflow at the mouth and nose. In partial airway obstruction, the inspiration or expiration is usually noisy by an inspiratory stridor or expiratory wheeze.<br> | ||
'''Breathing:''' Hypoxaemia is a reversible cause and after assessment and securing the airway, ventilation of the patient should be optimized. Arterial blood oxygen saturation can be monitored to assess hypoxaemia. If necessary tracheal intubation, sedation and controllered ventilation should be instituted.<br> | '''Breathing:''' Hypoxaemia is a reversible cause and after assessment and securing the airway, ventilation of the patient should be optimized. The airway can be secured using a variety of devices and ventilation methods. Arterial blood oxygen saturation can be monitored to assess hypoxaemia. If necessary tracheal intubation, sedation and controllered ventilation should be instituted.<br> | ||
'''Circulation:''' Myocardial ischemia or infarction is a common cause of cardiac arrest. Furthermore before or after the cardiac arrest tachycardias or bradycardias may occur and acute management is indicated. <br> | '''Circulation:''' Myocardial ischemia or infarction is a common cause of cardiac arrest. Furthermore before or after the cardiac arrest tachycardias or bradycardias may occur and acute management is indicated. <br> | ||
'''Disability:''' This step consist of determining the Glasgow Coma Scale of the patients and look for neurologic symptoms that might cause cardiac arrest. Furthermore it is important monitor glucose and temperature. <br> | '''Disability:''' This step consist of determining the Glasgow Coma Scale of the patients and look for neurologic symptoms that might cause cardiac arrest. Furthermore it is important monitor glucose and temperature. <br> | ||
| Line 44: | Line 43: | ||
====Shock protocol==== | ====Shock protocol==== | ||
When a shockable rhythm is detected, it is important to minimize the time between chest compressions and defibrillation. When the shock is delivered immediately resume with the chest compressions to minimize delay. Even after a successful shock the heart can be stunned and effective circulation can only be maintained through chest compressions. After the first round of shock and compressions reassess rhythm and act according to the protocol. After the third shock has been given, adrenaline 1mg and amiodarone 300mg can be administered intravenously. Further adrenaline 1mg can be administered every 3-5 minutes, there is no further indication for anti-arrhythmic drugs during resuscitation. Continuous monitoring is required for return of spontaneous circulation or for asystole and initiation of the no-shock protocol. | When a shockable rhythm is detected, it is important to minimize the time between chest compressions and defibrillation.<cite>Edelson, Eftestol</cite> When the shock is delivered immediately resume with the chest compressions to minimize delay. Even after a successful shock the heart can be stunned and effective circulation can only be maintained through chest compressions. After the first round of shock and compressions reassess rhythm and act according to the protocol. After the third shock has been given, adrenaline 1mg and amiodarone 300mg can be administered intravenously.<cite>Olasveengen, Dorian</cite> Further adrenaline 1mg can be administered every 3-5 minutes, there is no further indication for anti-arrhythmic drugs during resuscitation. Continuous monitoring is required for return of spontaneous circulation or for asystole and initiation of the no-shock protocol. | ||
====No-shock protocol==== | ====No-shock protocol==== | ||
When asystole or pulseless electrical activity is detected CPR should be started immediately simultaneously with 1mg intravenous adrenaline. Assess the rhythm after 2 minutes of chest compressions and continue according to the rhythm. Continue with adrenaline injections intravenously every 3-5 minutes if no return of spontaneous circulation has been achieved. There is no place for further medical intervention. | When asystole or pulseless electrical activity is detected CPR should be started immediately simultaneously with 1mg intravenous adrenaline. Assess the rhythm after 2 minutes of chest compressions and continue according to the rhythm. Continue with adrenaline injections intravenously every 3-5 minutes if no return of spontaneous circulation has been achieved. There is no place for further medical intervention. | ||
====Post-cardiac arrest treatment==== | ====Post-cardiac arrest treatment==== | ||
After cardiac arrest and return of spontaneous circulation the whole body ischemia/reperfusion affects all organ systems. Multiple organ failure, increased risk of infection, neurocognitive dysfunction and myocardial dysfunction are common problems encountered after a cardiac arrest which resembles the problems encountered with sepsis. After resuscitation strict control of oxygenation, cardiac output and glucose metabolism can improve outcome after cardiac arrest. Treatment of the underlying cause of the cardiac resuscitation, for instance a myocardial infarction should be considered. Studies have indicated that therapeutic hypothermia (32-34<sup>o</sup>C) during 12-24h after cardiac arrest can increase neurological outcome. This can be achieved by internal infusion or external cooling. Therapeutic hypothermia should be initiated in comatose patients quickly after return of circulation. When cooled the temperature should be maintained without to much fluctuations. Warming of the patient should occur very slowly (0.25<sup>o</sup>C to 0.5<sup>o</sup>C per hour) to prevent rapid plasma electrolyte concentration changes, intravascular volume and metabolic rate changes. | After cardiac arrest and return of spontaneous circulation the whole body ischemia/reperfusion affects all organ systems. Multiple organ failure, increased risk of infection, neurocognitive dysfunction and myocardial dysfunction are common problems encountered after a cardiac arrest which resembles the problems encountered with sepsis.<cite>Nolan5</cite> After resuscitation strict control of oxygenation, cardiac output and glucose metabolism can improve outcome after cardiac arrest.<cite>Balan,Nolan5,Padkin</cite> Treatment of the underlying cause of the cardiac resuscitation, for instance a myocardial infarction should be considered. Studies have indicated that therapeutic hypothermia (32-34<sup>o</sup>C) during 12-24h after cardiac arrest can increase neurological outcome.<cite>Froehler</cite> This can be achieved by internal infusion or external cooling. Therapeutic hypothermia should be initiated in comatose patients quickly after return of circulation. When cooled the temperature should be maintained without to much fluctuations.<cite>Polderman</cite> Warming of the patient should occur very slowly (0.25<sup>o</sup>C to 0.5<sup>o</sup>C per hour) to prevent rapid plasma electrolyte concentration changes, intravascular volume and metabolic rate changes.<cite>Arrich</cite> | ||
====Prognosis after cardiac arrest==== | ====Prognosis after cardiac arrest==== | ||
Prognosis after cardiac arrest is difficult and cannot be fully predicted. Survival after cardiac arrest is poor, mainly due to neurological damage, and two out of three patients admitted to the ICU following cardiac arrest die from neurological injury. Most prognostic markers have been studied in the era before therapeutic hypothermia. Therefore their value in patients that are actively cooled is incompletely understood. It is not possible to predict outcome reliable within 24 hours after cardiac arrest. Clinical examination of the patient can give information on the prognosis of the patient 24 hours after cardiac arrest. After 72 hours the absence of both pupillary light and corneal reflex predict poor outcome. In patients that are not treated with therapeutic hypothermia absence of vestibulo-ocular reflexes at >24h and a Glasgow coma scale motor score of 2 or less >72 hours after return of spontaneous circulation are possible prognostic markers of a worse outcome. Furthermore myoclonal status is associated with poor outcome, but recovery can occur, and is therefore not useful in determining the prognosis. Electrophysiological studies measuring somatosensory evoked potentials (SSEP) after 24 hours, absence of bilateral N20 cortical response to median nerve stimulation predicts a poor outcome. | Prognosis after cardiac arrest is difficult and cannot be fully predicted. Survival after cardiac arrest is poor, mainly due to neurological damage, and two out of three patients admitted to the ICU following cardiac arrest die from neurological injury.<cite>Laver</cite> Most prognostic markers have been studied in the era before therapeutic hypothermia. Therefore their value in patients that are actively cooled is incompletely understood. It is not possible to predict outcome reliable within 24 hours after cardiac arrest. Clinical examination of the patient can give information on the prognosis of the patient 24 hours after cardiac arrest. After 72 hours the absence of both pupillary light and corneal reflex predict poor outcome.<cite>Zandbergen</cite> In patients that are not treated with therapeutic hypothermia absence of vestibulo-ocular reflexes at >24h and a Glasgow coma scale motor score of 2 or less >72 hours after return of spontaneous circulation are possible prognostic markers of a worse outcome.<cite>Zandbergen, Edgren</cite> Furthermore myoclonal status is associated with poor outcome, but recovery can occur, and is therefore not useful in determining the prognosis.<cite>English</cite> Electrophysiological studies measuring somatosensory evoked potentials (SSEP) after 24 hours, absence of bilateral N20 cortical response to median nerve stimulation predicts a poor outcome.<cite>Wijdicks</cite> | ||
==Special circumstances== | ==Special circumstances== | ||
| Line 71: | Line 70: | ||
=References= | =References= | ||
<biblio> | <biblio> | ||
# ESC isbn=9780199566990 | #ESC isbn=9780199566990 | ||
# Nolan1 pmid=20956052 | #Nolan1 pmid=20956052 | ||
# Koster2 pmid=20956051 | #Koster2 pmid=20956051 | ||
# Deakin3 pmid=20956050 | #Deakin3 pmid=20956050 | ||
# Deakin4 pmid=20956049 | #Deakin4 pmid=20956049 | ||
# Soar8 pmid=20956045 | #Soar8 pmid=20956045 | ||
# Atwood pmid=16199289 | #Atwood pmid=16199289 | ||
# Meaney pmid=19770741 | #Meaney pmid=19770741 | ||
# Waalewijn pmid=11719156 | # Waalewijn pmid=11719156 | ||
# Holmberg1 pmid=11320981 | # Holmberg1 pmid=11320981 | ||
# Holmberg2 pmid=9547841 | # Holmberg2 pmid=9547841 | ||
# SOSKANTO pmid=17368153 | # SOSKANTO pmid=17368153 | ||
# White pmid=20026780 | # White pmid=20026780 | ||
# Peberdy pmid=16784998 | # Peberdy pmid=16784998 | ||
# Mejicano pmid=9841588 | # Mejicano pmid=9841588 | ||
# Fingerhut pmid=10662354 | # Fingerhut pmid=10662354 | ||
# Guildner pmid=1018395 | # Guildner pmid=1018395 | ||
# Ruben pmid=740619 | # Ruben pmid=740619 | ||
# Niemann pmid=10381988 | # Niemann pmid=10381988 | ||
| Line 102: | Line 101: | ||
# Mattu pmid=12098179 | # Mattu pmid=12098179 | ||
# Kornberger pmid=10488932 | # Kornberger pmid=10488932 | ||
# Reuler pmid=358883 | # Reuler pmid=358883 | ||
# Zell pmid=3985447 | # Zell pmid=3985447 | ||
# Pease pmid=12075060 | # Pease pmid=12075060 | ||
| Line 116: | Line 115: | ||
# Choo pmid=22513951 | # Choo pmid=22513951 | ||
# Sheikh pmid=17620060 | # Sheikh pmid=17620060 | ||
# Anthi pmid=9440561 | # Anthi pmid=9440561 | ||
# Pottle pmid=11886732 | # Pottle pmid=11886732 | ||
# elBanayosy pmid=9713724 | # elBanayosy pmid=9713724 | ||
| Line 130: | Line 129: | ||
# Geddes pmid=3543629 | # Geddes pmid=3543629 | ||
# Cooper pmid=8570929 | # Cooper pmid=8570929 | ||
# Smith pmid=15071378 | |||
# Hodgetts pmid=12161291 | |||
# Bellomo pmid=20598425 | |||
# Hillman pmid=15964445 | |||
# Pellis pmid=19010581 | |||
# Glaeser pmid=8517560 | |||
# Olasveengen pmid=19934423 | |||
# Nolan5 pmid=18963350 | |||
# Thim pmid=22319249 | |||
# Guly pmid=12835350 | |||
# Balan pmid=17068310 | |||
# Padkin pmid=19460604 | |||
# Froehler pmid=17559883 | |||
# Polderman pmid=19237924 | |||
# Arrich pmid=17334257 | |||
# Laver pmid=15365608 | |||
# Zandbergen pmid=16401847 | |||
# Edgren pmid=3621954 | |||
# English pmid=19604197 | |||
# Wijdicks pmid=16864809 | |||
# Edelson pmid=16982127 | |||
# Eftestol pmid=12010909 | |||
# Dorian pmid=11907287 | |||
# IHI http://www.ihi.org/knowledge/Pages/ImprovementStories/HospitalatNightProgram.aspx | # IHI http://www.ihi.org/knowledge/Pages/ImprovementStories/HospitalatNightProgram.aspx | ||
</biblio> | |||
Latest revision as of 09:33, 1 November 2023
Sébastien Krul, MD, Jonas de Jong, MD
Introduction
Survival of cardiac arrest continues to be very poor. In-hospital cardiac arrest has a survival to hospital discharge of 17,6% all rhythms[1]. Out-of-hospital cardiac arrest has a worse survival with 10,7% survival to hospital discharge for all rhythms.[2] Survival is dependent on the characteristics of the cardiac arrest (rhythm), on the patient’s medical history, and the time between the cardiac arrest en start of resuscitation.[3, 4, 5] The introduction of the automated external defibrillator (AED) has dramatically increased survival of out-of-hospital cardiac arrest victims.[6, 7] In this chapter we give an overview of basic life support (BLS) and advanced life support (ALS) based on the recommendation of the European Resuscitation Council Guidelines for Resuscitation 2010.
Basic Life Support (BLS)
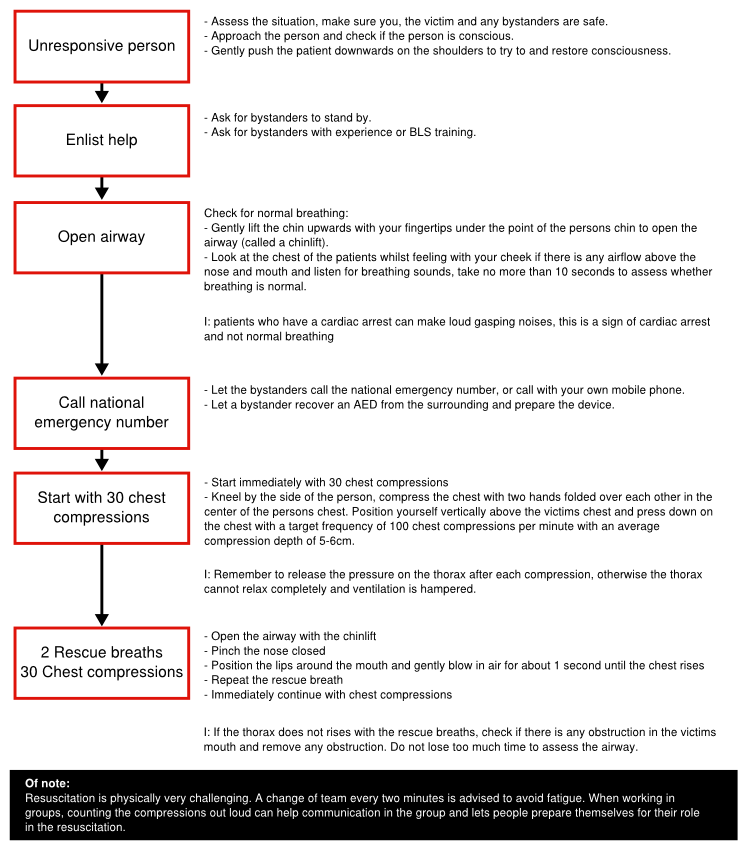
To increase survival after cardiac arrest it is vital to decrease the time to resuscitation.[3] The training of persons in BLS can increase bystander participation in performing cardiopulmonary resuscitation (CPR).[8] When non-arrest victims inadvertently receive CPR it is extremely rare to inflict serious harm (2% chance of a fracture)[9]. Furthermore the risk of disease transmission is extremely low, especially without high-risk activities as intravenous canulation.[10, 11] A straightforward protocol has been created to execute BLS (Figure 1).[12]
If at any stage the patient is conscious, has normal ventilation or recovers consciousness a care provider should find out what is wrong with the person and get help if needed. Repeated reassessment is necessary to detected deterioration of the patient’s condition.
Foreign body airway obstruction
An obstruction of the airway is uncommon, but reversible and adequate recognition can prevent cardiac arrest.[13] Airway obstruction is usually related to eating. In a mild obstruction patients can cough and speak and only frequent reassessment is advised. Patients that have a severe obstruction are unable to speak and have problems breathing and coughing. If a patient is still conscious five back blows can be applied between the shoulder blades whilst the patient leans forward. Otherwise five abdominal thrusts can be applied by clenching a fist and grasping it with the other hand. Place the hands it between the rib-cage and the umbilicus and pull sharply inward and upward whilst standing behind the patients.[14, 15] If the patient loses consciousness start BLS.[12]
Basic life support in children
In general the BLS algorithm is similar in children. However, due to the differences in underlying pathology of cardiac arrest and the size of children, small changes must be incorporated. Firstly, as pulmonary causes for cardiac arrest are more frequent, the BLS can be started with 5 initial rescue breaths before starting with the chest compression. The chest compression should compress the chest at least one third of the depth. The chest compression can be performed with one or two hands for a child over 1 year and with 2 fingers for an infant under 1 year.[12]
Automatic external defibrillator (AED)
The AED is a complex device that analyses the rhythm of patients and delivers a shock to defibrillate patients. It detect whether a patient has ventricular fibrillation or a different arrhythmia. When it detects a shockable rhythm it advises the user to deliver the shock, all settings are automatically adjusted. It also remembers the course of events so that the tracing can be recovered and analysed after the resuscitation.
When the AED is attached during BLS let the AED assess the rhythm. Do not manipulate the person while the AED assesses the rhythm to prevent motion artefact disturbing the detection algorithm. Follow the instructions of the AED; this can be either a shock or no shock. After shock or non-shock immediately continue with chest compressions and rescue breaths. Continue the CPR until the AED rechecks the rhythm. Standard AED are usable for children older than 8 years, special paediatric pads and an AED paediatric mode should be used in younger children.[16]
Preventing in Hosptial Cardiac Arrest
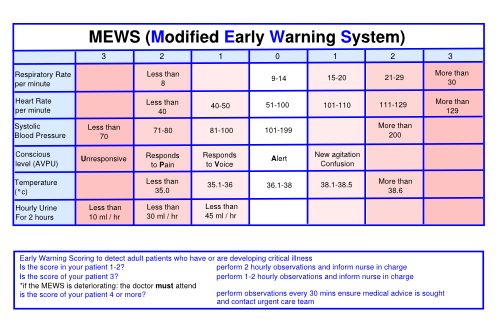
The best way to prevent sudden death is to early detect deterioration of a patient and to act on early warning signs.[18] Cardiac arrest is rarely unpredictable and is precipitated by a slow deterioration. An early warning score (Figure 2) helps to create consensus among care providers about the sickness of a patient.[19, 20] If the summed score reached a certain threshold, a doctor should be notified. The notified doctor should assess the patient within 30 minutes and discuss a treatment plan. If the patient does not improve within 60 minutes a reassessment should follow with possible inclusion of a medical emergency team (MET) or intensive care specialist.[21]
Advanced Life Support (ALS)
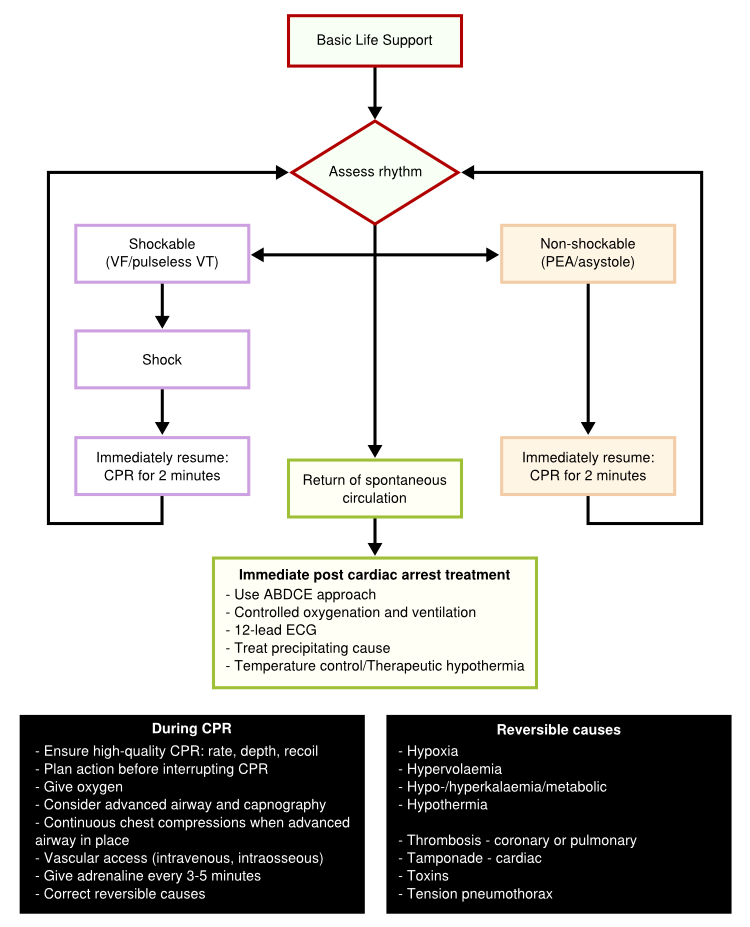
BLS the cornerstone to the treatment of cardiac arrest. Early and high quality CPR is critical to survival. In the hospital setting trained experts and technical equipment can facilitate cardiac arrest management. In case of a witnessed cardiac arrest caused by VT/VF in a monitored setting, three successive shocks followed by immediate CPR may be considered. If no defibrillation options are available and a precordial thump can be given in the first few seconds after the cardiac arrest.[22] It can not cause delay of the resuscitation attempt. The only intervention besides proper BLS and early defibrillation to increase survival is the administration of adrenaline.[23] The ALS protocol deviates into two strategies encountered in the setting of cardiac arrest; a shock protocol and no-shock protocol (Figure 3). During both protocols it is important to establish intravascular access as soon as possible, as an alternative intraosseous injection of drugs can be performed.[24] Furthermore assessment of airway management and ventilation is essential. Oxygen should be administered as soon as possible and be titrated to the arterial blood oxygen saturation. Tracheal intubation is the optimal method of providing and maintaining a clear and secure airway. Intubation should be performed by experienced personnel to reduce complications and delay between intubation and chest compressions. When there is return of spontaneous circulation the resuscitation team should stabilize the patient to prevent recurrence of cardiac arrest.[25, 26]
Patient assessment
During a cardiac arrest a structured assessment of the patient is required to detect the effects of the resuscitation, return of spontaneous circulation, reversible causes. To facilitate this assessment, an ABCDE approach can be used.[27, 28]
Airway: During the first step it is important to assess if the airway is clear. Airway obstruction can occur at any level. It can be caused by obstruction from the soft palate and epiglottis, blood, vomit and foreign bodies or airway oedema. It is important to look, listen and feel for airway obstruction. Look for chest and abdominal movements, listen and feel for airflow at the mouth and nose. In partial airway obstruction, the inspiration or expiration is usually noisy by an inspiratory stridor or expiratory wheeze.
Breathing: Hypoxaemia is a reversible cause and after assessment and securing the airway, ventilation of the patient should be optimized. The airway can be secured using a variety of devices and ventilation methods. Arterial blood oxygen saturation can be monitored to assess hypoxaemia. If necessary tracheal intubation, sedation and controllered ventilation should be instituted.
Circulation: Myocardial ischemia or infarction is a common cause of cardiac arrest. Furthermore before or after the cardiac arrest tachycardias or bradycardias may occur and acute management is indicated.
Disability: This step consist of determining the Glasgow Coma Scale of the patients and look for neurologic symptoms that might cause cardiac arrest. Furthermore it is important monitor glucose and temperature.
Environment: In an out of hospital cardiac arrest setting it is important to secure the environment of the cardiac arrest. There should be a safe environment for both the caregiver and the patient. The patient and environment itself might show the cause of the cardiac arrest e.g. chemical or electrical burns, drowning, anaphylactic shock, illicit drugs.
Shock protocol
When a shockable rhythm is detected, it is important to minimize the time between chest compressions and defibrillation.[29, 30] When the shock is delivered immediately resume with the chest compressions to minimize delay. Even after a successful shock the heart can be stunned and effective circulation can only be maintained through chest compressions. After the first round of shock and compressions reassess rhythm and act according to the protocol. After the third shock has been given, adrenaline 1mg and amiodarone 300mg can be administered intravenously.[23, 31] Further adrenaline 1mg can be administered every 3-5 minutes, there is no further indication for anti-arrhythmic drugs during resuscitation. Continuous monitoring is required for return of spontaneous circulation or for asystole and initiation of the no-shock protocol.
No-shock protocol
When asystole or pulseless electrical activity is detected CPR should be started immediately simultaneously with 1mg intravenous adrenaline. Assess the rhythm after 2 minutes of chest compressions and continue according to the rhythm. Continue with adrenaline injections intravenously every 3-5 minutes if no return of spontaneous circulation has been achieved. There is no place for further medical intervention.
Post-cardiac arrest treatment
After cardiac arrest and return of spontaneous circulation the whole body ischemia/reperfusion affects all organ systems. Multiple organ failure, increased risk of infection, neurocognitive dysfunction and myocardial dysfunction are common problems encountered after a cardiac arrest which resembles the problems encountered with sepsis.[26] After resuscitation strict control of oxygenation, cardiac output and glucose metabolism can improve outcome after cardiac arrest.[26, 32, 33] Treatment of the underlying cause of the cardiac resuscitation, for instance a myocardial infarction should be considered. Studies have indicated that therapeutic hypothermia (32-34oC) during 12-24h after cardiac arrest can increase neurological outcome.[34] This can be achieved by internal infusion or external cooling. Therapeutic hypothermia should be initiated in comatose patients quickly after return of circulation. When cooled the temperature should be maintained without to much fluctuations.[35] Warming of the patient should occur very slowly (0.25oC to 0.5oC per hour) to prevent rapid plasma electrolyte concentration changes, intravascular volume and metabolic rate changes.[36]
Prognosis after cardiac arrest
Prognosis after cardiac arrest is difficult and cannot be fully predicted. Survival after cardiac arrest is poor, mainly due to neurological damage, and two out of three patients admitted to the ICU following cardiac arrest die from neurological injury.[37] Most prognostic markers have been studied in the era before therapeutic hypothermia. Therefore their value in patients that are actively cooled is incompletely understood. It is not possible to predict outcome reliable within 24 hours after cardiac arrest. Clinical examination of the patient can give information on the prognosis of the patient 24 hours after cardiac arrest. After 72 hours the absence of both pupillary light and corneal reflex predict poor outcome.[38] In patients that are not treated with therapeutic hypothermia absence of vestibulo-ocular reflexes at >24h and a Glasgow coma scale motor score of 2 or less >72 hours after return of spontaneous circulation are possible prognostic markers of a worse outcome.[38, 39] Furthermore myoclonal status is associated with poor outcome, but recovery can occur, and is therefore not useful in determining the prognosis.[40] Electrophysiological studies measuring somatosensory evoked potentials (SSEP) after 24 hours, absence of bilateral N20 cortical response to median nerve stimulation predicts a poor outcome.[41]
Special circumstances
In all circumstances the normal protocol for BLS and ALS is the cornerstone in the treatment of cardiac arrest. However some conditions encountered during resuscitation or as a cause of cardiac arrest, can affect the procedure.[42]
- Anaphylaxis: Anaphylaxis is a life-threatening hypersensitivity reaction and can be accompanied by airway/breathing/circulation problems due to swelling of the mucosa.[43] The cause of the anaphylaxis should be identified and can be a broad range of triggers (food, insects, drugs etc.).[44] Anaphylaxis rapidly develops after exposure to the trigger, usually within minutes. Patients should receive intramuscular adrenaline before an intravenous route is established and anti-inflammatory drugs (steroids, anti-histamines) should be initiated.[44, 45, 46, 47] Oxygen en fluids should be administered as swelling of the airway can result impair breathing and due to fluid loss is out of the circulation hypovolaemia can develop.
- Asthma: Patients with asthma who experience a cardiac arrest usually have a long period of hypoxaemia, however cardiac arrest is not necessarily related to asthma severity.[48] Patients with acute severe asthma require oxygen, aggressive medical therapy and should be admitted to the critical care area. The main troubles encountered in the resuscitation of patients with asthma relates to the underlying lung disease. In general increased lung resistance makes ventilation of these patients difficult and can increase the risk of gastric inflation.[49] Early intubation is indicated in these patients during the ALS setting. Due to the hyperinflation of the lungs more energy might be required in defibrillating these patients, as the heart is isolated by air.[50]
- Cardiac arrest after cardiac surgery: Cardiac arrest after cardiac surgery is usually caused by specific causes related as a consequence of the cardiac surgery, such as tamponade, hypovolaemia, myocardial ischaemia, tension pneumothorax, or pacing failure.[51] Early resternotomy can be the key to survival, especially after repeated defibrillation has failed or if asystole is observed.[52, 53, 54] When the sternum is opened internal cardioversion (output of 5-20J) and cardiac compression can be applied across the ventricles.
- Drowning: Drowning is a common cause of accidental death.[55] There are no differences between victims of salt water and fresh water drowning. Correction of hypoxia is critical in the outcome of these victims as cardiac arrest is a consequence of the hypoxia. Care should be taken to start immediate resuscitation and restore oxygenation, ventilation and perfusion. During BLS it is recommended to start the BLS with 5 rescue breaths.[56] Rescue breathing is difficult after drowning due tot the presence of fluid in the airway and the high inflation pressure required after drowning. Furthermore regurgitation is common and removal of the regurgitated material during resuscitation is required.[57] It is common for hypothermia to be present in victims of drowning, complicating the resuscitation attempt. After return of spontaneous circulation, pneumonia is common and patients are prone to develop acute respiratory distress syndrome (ARDS).[58, 59]
- Electrocution: Electrocution can result in multi-system injury and usually occur in the workspace in adult or at home in children. The direct effects of an electric shock on tissues, for instance paralysis of the respiratory system or muscles, VF in the myocardium, ischemia due to coronary artery spasm or asystole can result in a cardiac arrest.[60] Electrical burns can complicate the resuscitation and care should be taken to avoid further complications resulting from these burns. Adequate fluid therapy is required if there is significant tissue destruction. Due to electrical burns around the neck and muscular paralysis early intubation and prolonged ventilatory support may be required.[61]
- Electrolyte disorder: Electrolyte abnormalities are among the most common causes of cardiac arrhythmias. Potassium disorders are commonly seen, especially hyperkalaemia has a high risk of malignant arrhythmias.[62] During cardiac arrest treatment of these abnormalities is no different than in the normal clinical setting, and aggressive treatment of the electrolyte disorder should be initiated.[63, 64]
- Hyperthermia: Exogenous or endogenous hyperthermia can result in heat stress, progressing to heat exhaustion and results in heat stroke.[65] Heat stress can provoke edema, syncope and cramps and is treated with rest, cooling and oral rehydration and salt replacement. Heat exhaustion is a systemic reaction to prolonged heat exposure and is accompanied by headaches, dizziness, nausea, vomiting, tachycardia, hypotension, muscle pain, weakness and cramps. Treatment is similar as in a heat stroke, but active cooling might be required in severe cases with ice packs or cold intravenous fluids. Heat stroke is a systemic inflammatory response with a core temperature above 40,6oC. It can lead to varying levels of organ dysfunction accompanied by mental changes.[66] It can occur during high environmental temperatures or during strenuous physical exercise in high environmental temperatures. Rapid cooling of the victim should occur as soon as possible.[67] Patients with heat-stroke usually have electrolyte abnormalities and hypovolaemia.
- Hypothermia: In hypothermia (<35oC) it is difficult to detect signs of life. Therefore resuscitation should proceed according to standard protocols until the patient has reached normothermia. Second to resuscitation, warming of the body temperature by passive or active external and internal methods should be started. Examples of passive rewarming are drying and insulation of the body, whilst examples of active rewarming are infusion of warmed intravenous fluids or forced air rewarming.[68, 69, 70] As a result of rewarming vasodilatation occurs and fluid administration may be required. Resuscitation during hypothermia is difficult, the thorax is stiff and the heart is less responsive to medication and defibrillation. Furthermore drug metabolism is slowed, resulting in increased plasma levels of medication.[71] Medication should be administered at double intervals in patients <35oC and withheld in patient <30oC. Rhythm disturbances usually seen at rewarming after hypothermia are bradycardia, atrial fibrillation, VF and asystole. Bradycardia and atrial fibrillation revert to normal sinus rhythm as the core body temperature increases.[72]
- Poisoning: Accidental poisoning in children or by therapeutic or recreational drugs in adults are the main causes of poisoning, however rarely causes cardiac arrest.[73] It is important to identify the poison to start antidote treatment or decontamination.[74] During the BLS and ALS care should be taken when performing mount-to-mouth ventilation in the presence of certain chemical types of poisoning. Respiratory arrest and airway depression is more common after poisoning.[75] Early intubation can prevent cardiac arrest and pulmonary aspiration. When confronted with a poisoning in an ALS setting, temperature should be monitored as hypo- or hyperthermia my occur after drug overdose. Furthermore, due to the slow metabolization or excretion of certain poisons the resuscitation can continue for a long period.
- Pregnancy: If a cardiac arrest occurs during pregnancy the safety of the fetus should always be considered. Due to the growth of the uterus compression of the inferior vena cava can occur and as a result venous return and cardiac output is compromised. During CPR displace the uterus to the left or apply a left lateral tilt of the surface the patient is lying upon to minimize compression from the uterus.[76] Furthermore the increased abdominal pressure can increase the risk of pulmonary aspiration and can hamper proper ventilation; therefore early intubation can lower risks and ease cardiopulmonary resuscitation. During ALS normal defibrillator shock energies can be used.[77] An emergency hysterotomy or cesarean section needs to be considered, if gestational age is after 20 weeks.[78] After 20 weeks the size of the uterus is large enough to compromise cardiac output, however fetal viability begins at approximately 24-25 weeks.[79]
- Traumatic Cardiorespiratory Arrest: Cardiac arrest caused by trauma has low chance of survival.[80] Blunt trauma can cause commotio cordis if there is an impact to the chest wall over the heart.[81] This impact can cause arrhythmias (usually ventricular fibrillation) and occurs often during sports.[82] Penetrating trauma can be cause for an emergency thoracotomy. Emergency thoracotomy has to be performed early after onset of CPR.[83] It is important to manage the resuscitation according to protocol and treat reversible causes.
References
- Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, and Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010 Jan;38(1):101-8. DOI:10.1097/CCM.0b013e3181b43282 |
- Atwood C, Eisenberg MS, Herlitz J, and Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005 Oct;67(1):75-80. DOI:10.1016/j.resuscitation.2005.03.021 |
- Waalewijn RA, Tijssen JG, and Koster RW. Bystander initiated actions in out-of-hospital cardiopulmonary resuscitation: results from the Amsterdam Resuscitation Study (ARRESUST). Resuscitation. 2001 Sep;50(3):273-9. DOI:10.1016/s0300-9572(01)00354-9 |
- Holmberg M, Holmberg S, Herlitz J, and Swedish Cardiac Arrest Registry. Factors modifying the effect of bystander cardiopulmonary resuscitation on survival in out-of-hospital cardiac arrest patients in Sweden. Eur Heart J. 2001 Mar;22(6):511-9. DOI:10.1053/euhj.2000.2421 |
- Holmberg M, Holmberg S, Herlitz J, and Gårdelöv B. Survival after cardiac arrest outside hospital in Sweden. Swedish Cardiac Arrest Registry. Resuscitation. 1998 Jan;36(1):29-36. DOI:10.1016/s0300-9572(97)00089-0 |
- ISBN:9780199566990
- Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B, and ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010 Oct;81(10):1219-76. DOI:10.1016/j.resuscitation.2010.08.021 |
- SOS-KANTO study group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet. 2007 Mar 17;369(9565):920-6. DOI:10.1016/S0140-6736(07)60451-6 |
- Peberdy MA, Ottingham LV, Groh WJ, Hedges J, Terndrup TE, Pirrallo RG, Mann NC, Sehra R, and PAD Investigators. Adverse events associated with lay emergency response programs: the public access defibrillation trial experience. Resuscitation. 2006 Jul;70(1):59-65. DOI:10.1016/j.resuscitation.2005.10.030 |
- Mejicano GC and Maki DG. Infections acquired during cardiopulmonary resuscitation: estimating the risk and defining strategies for prevention. Ann Intern Med. 1998 Nov 15;129(10):813-28. DOI:10.7326/0003-4819-129-10-199811150-00014 |
- Koster RW, Baubin MA, Bossaert LL, Caballero A, Cassan P, Castrén M, Granja C, Handley AJ, Monsieurs KG, Perkins GD, Raffay V, and Sandroni C. European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010 Oct;81(10):1277-92. DOI:10.1016/j.resuscitation.2010.08.009 |
- Fingerhut LA, Cox CS, and Warner M. International comparative analysis of injury mortality. Findings from the ICE on injury statistics. International Collaborative Effort on Injury Statistics. Adv Data. 1998 Oct 7(303):1-20.
- Guildner CW, Williams D, and Subitch T. Airway obstructed by foreign material: the Heimlich maneuver. JACEP. 1976 Sep;5(9):675-7. DOI:10.1016/s0361-1124(76)80099-8 |
- Ruben H and Macnaughton FI. The treatment of food-choking. Practitioner. 1978 Nov;221(1325):725-9.
- Deakin CD, Nolan JP, Sunde K, and Koster RW. European Resuscitation Council Guidelines for Resuscitation 2010 Section 3. Electrical therapies: automated external defibrillators, defibrillation, cardioversion and pacing. Resuscitation. 2010 Oct;81(10):1293-304. DOI:10.1016/j.resuscitation.2010.08.008 |
- Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, Silvester W, Doolan L, and Gutteridge G. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004 Apr;32(4):916-21. DOI:10.1097/01.ccm.0000119428.02968.9e |
- Hodgetts TJ, Kenward G, Vlachonikolis IG, Payne S, and Castle N. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation. 2002 Aug;54(2):125-31. DOI:10.1016/s0300-9572(02)00100-4 |
- Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, Finfer S, Flabouris A, and MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005 Jun 18-24;365(9477):2091-7. DOI:10.1016/S0140-6736(05)66733-5 |
- Smith GB. In-hospital cardiac arrest: is it time for an in-hospital 'chain of prevention'?. Resuscitation. 2010 Sep;81(9):1209-11. DOI:10.1016/j.resuscitation.2010.04.017 |
- Pellis T, Kette F, Lovisa D, Franceschino E, Magagnin L, Mercante WP, and Kohl P. Utility of pre-cordial thump for treatment of out of hospital cardiac arrest: a prospective study. Resuscitation. 2009 Jan;80(1):17-23. DOI:10.1016/j.resuscitation.2008.10.018 |
- Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, and Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009 Nov 25;302(20):2222-9. DOI:10.1001/jama.2009.1729 |
- Glaeser PW, Hellmich TR, Szewczuga D, Losek JD, and Smith DS. Five-year experience in prehospital intraosseous infusions in children and adults. Ann Emerg Med. 1993 Jul;22(7):1119-24. DOI:10.1016/s0196-0644(05)80975-8 |
- Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, and Perkins GD. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation. 2010 Oct;81(10):1305-52. DOI:10.1016/j.resuscitation.2010.08.017 |
- Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, and Hoek TV. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation. 2008 Dec;79(3):350-79. DOI:10.1016/j.resuscitation.2008.09.017 |
- Thim T, Krarup NH, Grove EL, Rohde CV, and Løfgren B. Initial assessment and treatment with the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach. Int J Gen Med. 2012;5:117-21. DOI:10.2147/IJGM.S28478 |
- Guly HR. ABCDEs. Emerg Med J. 2003 Jul;20(4):358. DOI:10.1136/emj.20.4.358 |
- Edelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM, Merchant RM, Hoek TL, Steen PA, and Becker LB. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006 Nov;71(2):137-45. DOI:10.1016/j.resuscitation.2006.04.008 |
- Eftestøl T, Sunde K, and Steen PA. Effects of interrupting precordial compressions on the calculated probability of defibrillation success during out-of-hospital cardiac arrest. Circulation. 2002 May 14;105(19):2270-3. DOI:10.1161/01.cir.0000016362.42586.fe |
- Dorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, and Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med. 2002 Mar 21;346(12):884-90. DOI:10.1056/NEJMoa013029 |
- Balan IS, Fiskum G, Hazelton J, Cotto-Cumba C, and Rosenthal RE. Oximetry-guided reoxygenation improves neurological outcome after experimental cardiac arrest. Stroke. 2006 Dec;37(12):3008-13. DOI:10.1161/01.STR.0000248455.73785.b1 |
- Padkin A. Glucose control after cardiac arrest. Resuscitation. 2009 Jun;80(6):611-2. DOI:10.1016/j.resuscitation.2009.04.019 |
- Froehler MT and Geocadin RG. Hypothermia for neuroprotection after cardiac arrest: mechanisms, clinical trials and patient care. J Neurol Sci. 2007 Oct 15;261(1-2):118-26. DOI:10.1016/j.jns.2007.04.042 |
- Polderman KH and Herold I. Therapeutic hypothermia and controlled normothermia in the intensive care unit: practical considerations, side effects, and cooling methods. Crit Care Med. 2009 Mar;37(3):1101-20. DOI:10.1097/CCM.0b013e3181962ad5 |
- Arrich J and European Resuscitation Council Hypothermia After Cardiac Arrest Registry Study Group. Clinical application of mild therapeutic hypothermia after cardiac arrest. Crit Care Med. 2007 Apr;35(4):1041-7. DOI:10.1097/01.CCM.0000259383.48324.35 |
- Laver S, Farrow C, Turner D, and Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004 Nov;30(11):2126-8. DOI:10.1007/s00134-004-2425-z |
- Zandbergen EG, Hijdra A, Koelman JH, Hart AA, Vos PE, Verbeek MM, de Haan RJ, and PROPAC Study Group. Prediction of poor outcome within the first 3 days of postanoxic coma. Neurology. 2006 Jan 10;66(1):62-8. DOI:10.1212/01.wnl.0000191308.22233.88 |
- Edgren E, Hedstrand U, Nordin M, Rydin E, and Ronquist G. Prediction of outcome after cardiac arrest. Crit Care Med. 1987 Sep;15(9):820-5. DOI:10.1097/00003246-198709000-00004 |
- English WA, Giffin NJ, and Nolan JP. Myoclonus after cardiac arrest: pitfalls in diagnosis and prognosis. Anaesthesia. 2009 Aug;64(8):908-11. DOI:10.1111/j.1365-2044.2009.05939.x |
- Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S, and Quality Standards Subcommittee of the American Academy of Neurology. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006 Jul 25;67(2):203-10. DOI:10.1212/01.wnl.0000227183.21314.cd |
- Soar J, Perkins GD, Abbas G, Alfonzo A, Barelli A, Bierens JJ, Brugger H, Deakin CD, Dunning J, Georgiou M, Handley AJ, Lockey DJ, Paal P, Sandroni C, Thies KC, Zideman DA, and Nolan JP. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010 Oct;81(10):1400-33. DOI:10.1016/j.resuscitation.2010.08.015 |
- Soar J, Pumphrey R, Cant A, Clarke S, Corbett A, Dawson P, Ewan P, Foëx B, Gabbott D, Griffiths M, Hall J, Harper N, Jewkes F, Maconochie I, Mitchell S, Nasser S, Nolan J, Rylance G, Sheikh A, Unsworth DJ, Warrell D, and Working Group of the Resuscitation Council (UK). Emergency treatment of anaphylactic reactions--guidelines for healthcare providers. Resuscitation. 2008 May;77(2):157-69. DOI:10.1016/j.resuscitation.2008.02.001 |
- Lieberman P, Camargo CA Jr, Bohlke K, Jick H, Miller RL, Sheikh A, and Simons FE. Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006 Nov;97(5):596-602. DOI:10.1016/S1081-1206(10)61086-1 |
- Kemp SF, Lockey RF, Simons FE, and World Allergy Organization ad hoc Committee on Epinephrine in Anaphylaxis. Epinephrine: the drug of choice for anaphylaxis. A statement of the World Allergy Organization. Allergy. 2008 Aug;63(8):1061-70. DOI:10.1111/j.1398-9995.2008.01733.x |
- Sheikh A, Ten Broek V, Brown SG, and Simons FE. H1-antihistamines for the treatment of anaphylaxis: Cochrane systematic review. Allergy. 2007 Aug;62(8):830-7. DOI:10.1111/j.1398-9995.2007.01435.x |
- Choo KJ, Simons FE, and Sheikh A. Glucocorticoids for the treatment of anaphylaxis. Cochrane Database Syst Rev. 2012 Apr 18;2012(4):CD007596. DOI:10.1002/14651858.CD007596.pub3 |
- Romagnoli M, Caramori G, Braccioni F, Ravenna F, Barreiro E, Siafakas NM, Vignola AM, Chanez P, Fabbri LM, Papi A, and ENFUMOSA Study Group. Near-fatal asthma phenotype in the ENFUMOSA Cohort. Clin Exp Allergy. 2007 Apr;37(4):552-7. DOI:10.1111/j.1365-2222.2007.02683.x |
-
pmid= 7618786
- Deakin CD, McLaren RM, Petley GW, Clewlow F, and Dalrymple-Hay MJ. Effects of positive end-expiratory pressure on transthoracic impedance--implications for defibrillation. Resuscitation. 1998 Apr;37(1):9-12. DOI:10.1016/s0300-9572(98)00049-5 |
- Anthi A, Tzelepis GE, Alivizatos P, Michalis A, Palatianos GM, and Geroulanos S. Unexpected cardiac arrest after cardiac surgery: incidence, predisposing causes, and outcome of open chest cardiopulmonary resuscitation. Chest. 1998 Jan;113(1):15-9. DOI:10.1378/chest.113.1.15 |
- Pottle A, Bullock I, Thomas J, and Scott L. Survival to discharge following open chest cardiac compression (OCCC). A 4-year retrospective audit in a cardiothoracic specialist centre--Royal Brompton and Harefield NHS Trust, United Kingdom. Resuscitation. 2002 Mar;52(3):269-72. DOI:10.1016/s0300-9572(01)00479-8 |
- el-Banayosy A, Brehm C, Kizner L, Hartmann D, Körtke H, Körner MM, Minami K, Reichelt W, and Körfer R. Cardiopulmonary resuscitation after cardiac surgery: a two-year study. J Cardiothorac Vasc Anesth. 1998 Aug;12(4):390-2. DOI:10.1016/s1053-0770(98)90189-6 |
- Dunning J, Fabbri A, Kolh PH, Levine A, Lockowandt U, Mackay J, Pavie AJ, Strang T, Versteegh MI, Nashef SA, and EACTS Clinical Guidelines Committee. Guideline for resuscitation in cardiac arrest after cardiac surgery. Eur J Cardiothorac Surg. 2009 Jul;36(1):3-28. DOI:10.1016/j.ejcts.2009.01.033 |
- Manolios N and Mackie I. Drowning and near-drowning on Australian beaches patrolled by life-savers: a 10-year study, 1973-1983. Med J Aust. 1988 Feb 15;148(4):165-7, 170-1.
- Gregorakos L, Markou N, Psalida V, Kanakaki M, Alexopoulou A, Sotiriou E, Damianos A, and Myrianthefs P. Near-drowning: clinical course of lung injury in adults. Lung. 2009 Mar-Apr;187(2):93-7. DOI:10.1007/s00408-008-9132-4 |
- van Berkel M, Bierens JJ, Lie RL, de Rooy TP, Kool LJ, van de Velde EA, and Meinders AE. Pulmonary oedema, pneumonia and mortality in submersion victims; a retrospective study in 125 patients. Intensive Care Med. 1996 Feb;22(2):101-7. DOI:10.1007/BF01720715 |
- Geddes LA, Bourland JD, and Ford G. The mechanism underlying sudden death from electric shock. Med Instrum. 1986 Nov-Dec;20(6):303-15.
- Cooper MA. Emergent care of lightning and electrical injuries. Semin Neurol. 1995 Sep;15(3):268-78. DOI:10.1055/s-2008-1041032 |
- Niemann JT and Cairns CB. Hyperkalemia and ionized hypocalcemia during cardiac arrest and resuscitation: possible culprits for postcountershock arrhythmias?. Ann Emerg Med. 1999 Jul;34(1):1-7. DOI:10.1016/s0196-0644(99)70265-9 |
- Alfonzo AV, Isles C, Geddes C, and Deighan C. Potassium disorders--clinical spectrum and emergency management. Resuscitation. 2006 Jul;70(1):10-25. DOI:10.1016/j.resuscitation.2005.11.002 |
- Mahoney BA, Smith WA, Lo DS, Tsoi K, Tonelli M, and Clase CM. Emergency interventions for hyperkalaemia. Cochrane Database Syst Rev. 2005 Apr 18;2005(2):CD003235. DOI:10.1002/14651858.CD003235.pub2 |
- Pease S, Bouadma L, Kermarrec N, Schortgen F, Régnier B, and Wolff M. Early organ dysfunction course, cooling time and outcome in classic heatstroke. Intensive Care Med. 2009 Aug;35(8):1454-8. DOI:10.1007/s00134-009-1500-x |
- Bouchama A and Knochel JP. Heat stroke. N Engl J Med. 2002 Jun 20;346(25):1978-88. DOI:10.1056/NEJMra011089 |
- Bouchama A, Dehbi M, and Chaves-Carballo E. Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care. 2007;11(3):R54. DOI:10.1186/cc5910 |
- Kornberger E, Schwarz B, Lindner KH, and Mair P. Forced air surface rewarming in patients with severe accidental hypothermia. Resuscitation. 1999 Jul;41(2):105-11. DOI:10.1016/s0300-9572(99)00069-6 |
- Reuler JB. Hypothermia: pathophysiology, clinical settings, and management. Ann Intern Med. 1978 Oct;89(4):519-27. DOI:10.7326/0003-4819-89-4-519 |
- Zell SC and Kurtz KJ. Severe exposure hypothermia: a resuscitation protocol. Ann Emerg Med. 1985 Apr;14(4):339-45. DOI:10.1016/s0196-0644(85)80101-3 |
- Paal P, Beikircher W, and Brugger H. [Avalanche emergencies. Review of the current situation]. Anaesthesist. 2006 Mar;55(3):314-24. DOI:10.1007/s00101-006-0997-4 |
- Mattu A, Brady WJ, and Perron AD. Electrocardiographic manifestations of hypothermia. Am J Emerg Med. 2002 Jul;20(4):314-26. DOI:10.1053/ajem.2002.32633 |
- Bronstein AC, Spyker DA, Cantilena LR Jr, Green JL, Rumack BH, and Giffin SL. 2008 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 26th Annual Report. Clin Toxicol (Phila). 2009 Dec;47(10):911-1084. DOI:10.3109/15563650903438566 |
- Zimmerman JL. Poisonings and overdoses in the intensive care unit: general and specific management issues. Crit Care Med. 2003 Dec;31(12):2794-801. DOI:10.1097/01.CCM.0000100123.50896.F0 |
- Yanagawa Y, Sakamoto T, and Okada Y. Recovery from a psychotropic drug overdose tends to depend on the time from ingestion to arrival, the Glasgow Coma Scale, and a sign of circulatory insufficiency on arrival. Am J Emerg Med. 2007 Sep;25(7):757-61. DOI:10.1016/j.ajem.2006.12.006 |
- Bamber JH and Dresner M. Aortocaval compression in pregnancy: the effect of changing the degree and direction of lateral tilt on maternal cardiac output. Anesth Analg. 2003 Jul;97(1):256-8, table of contents. DOI:10.1213/01.ane.0000067400.79654.30 |
- Nanson J, Elcock D, Williams M, and Deakin CD. Do physiological changes in pregnancy change defibrillation energy requirements?. Br J Anaesth. 2001 Aug;87(2):237-9. DOI:10.1093/bja/87.2.237 |
- Katz V, Balderston K, and DeFreest M. Perimortem cesarean delivery: were our assumptions correct?. Am J Obstet Gynecol. 2005 Jun;192(6):1916-20; discussion 1920-1. DOI:10.1016/j.ajog.2005.02.038 |
- Allen MC, Donohue PK, and Dusman AE. The limit of viability--neonatal outcome of infants born at 22 to 25 weeks' gestation. N Engl J Med. 1993 Nov 25;329(22):1597-601. DOI:10.1056/NEJM199311253292201 |
- Rosemurgy AS, Norris PA, Olson SM, Hurst JM, and Albrink MH. Prehospital traumatic cardiac arrest: the cost of futility. J Trauma. 1993 Sep;35(3):468-73; discussion 473-4.
- Maron BJ and Estes NA 3rd. Commotio cordis. N Engl J Med. 2010 Mar 11;362(10):917-27. DOI:10.1056/NEJMra0910111 |
- Maron BJ, Doerer JJ, Haas TS, Tierney DM, and Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009 Mar 3;119(8):1085-92. DOI:10.1161/CIRCULATIONAHA.108.804617 |
- Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons. Committee on Trauma. Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg. 2001 Sep;193(3):303-9. DOI:10.1016/s1072-7515(01)00999-1 |
- White L, Rogers J, Bloomingdale M, Fahrenbruch C, Culley L, Subido C, Eisenberg M, and Rea T. Dispatcher-assisted cardiopulmonary resuscitation: risks for patients not in cardiac arrest. Circulation. 2010 Jan 5;121(1):91-7. DOI:10.1161/CIRCULATIONAHA.109.872366 |
- Youn CS, Choi SP, Yim HW, and Park KN. Out-of-hospital cardiac arrest due to drowning: An Utstein Style report of 10 years of experience from St. Mary's Hospital. Resuscitation. 2009 Jul;80(7):778-83. DOI:10.1016/j.resuscitation.2009.04.007 |
- Simpson CR and Sheikh A. Adrenaline is first line treatment for the emergency treatment of anaphylaxis. Resuscitation. 2010 Jun;81(6):641-2. DOI:10.1016/j.resuscitation.2010.04.002 |