Chest Pain / Angina Pectoris: Difference between revisions
Secretariat (talk | contribs) No edit summary |
Secretariat (talk | contribs) No edit summary |
||
| Line 32: | Line 32: | ||
===Additional Research=== | ===Additional Research=== | ||
If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done.<cite> | If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done.<cite>Fox</cite> Depending on the hospital one of the below standing research will be done. | ||
# Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity.<cite>Amanullah</cite> | # Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity.<cite>Amanullah</cite> | ||
# Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest.<cite>Brown</cite> | # Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest.<cite>Brown</cite> | ||
| Line 41: | Line 41: | ||
==Coronary Angiography== | ==Coronary Angiography== | ||
In patients with unstable angina pectoris early coronary angiography possibly followed by revascularization is usually performed within 4 to 24 hours of admission in the hospital. In most clinical trials this strategy has shown a reduction in the incidence of death or nonfatal myocardial infraction.<cite> | In patients with unstable angina pectoris early coronary angiography possibly followed by revascularization is usually performed within 4 to 24 hours of admission in the hospital. In most clinical trials this strategy has shown a reduction in the incidence of death or nonfatal myocardial infraction.<cite>Anderson</cite> | ||
A CAG is an X ray examination of the coronary arteries, a catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. Contrast is visible by X ray and the images that are obtained are called angiograms. | A CAG is an X ray examination of the coronary arteries, a catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. Contrast is visible by X ray and the images that are obtained are called angiograms. | ||
| Line 51: | Line 51: | ||
In patients with stable angina pectoris percutaneous coronary intervention does not offer any benefit in terms of death, myocardial infarction, or the need for subsequent revascularization compared with conservative medical treatment.<cite>Katritsis</cite> | In patients with stable angina pectoris percutaneous coronary intervention does not offer any benefit in terms of death, myocardial infarction, or the need for subsequent revascularization compared with conservative medical treatment.<cite>Katritsis</cite> | ||
Initial treatment of stable angina pectoris therefore focuses on medication to keep the workload of the heart as low as possible. β blockers lower heart rate and blood pressure, this decreases the oxygen demand of the heart.<cite>Garcia</cite> Nitrates dilatate the coronary arteries so the heart receives more oxygenated blood.<cite> | Initial treatment of stable angina pectoris therefore focuses on medication to keep the workload of the heart as low as possible. β blockers lower heart rate and blood pressure, this decreases the oxygen demand of the heart.<cite>Garcia</cite> Nitrates dilatate the coronary arteries so the heart receives more oxygenated blood.<cite>Abrams</cite> Anticoagulants (aspirin) to reduce the risk of development of a thrombus in the coronary arteries.<cite>Hennekens</cite> | ||
Apart from starting medication the patient needs to minimize any present risk factors like smoking, overweight and drinking alcohol. ''See chronic coronary diseases''. | Apart from starting medication the patient needs to minimize any present risk factors like smoking, overweight and drinking alcohol. ''See chronic coronary diseases''. | ||
| Line 92: | Line 92: | ||
==History== | ==History== | ||
Classic presentation of a myocardial infarction is acute chest pain which lasts longer than a few minutes. | Classic presentation of a myocardial infarction is acute chest pain which lasts longer than a few minutes.<cite>Swap</cite> The pain does not decrease at rest and is only temporarily relieved with nitroglycerin. Common accompanying symptoms are radiating pain to shoulder, arm, back and/or jaw.<cite>Foreman</cite> Shortness of breath can occur, as well as sweating, fainting, nausea and vomiting, so called vegetative symptoms. Some patients not really complain about chest pain but more about abdominal pain so as with angina pectoris the presentation can be very a specific.<cite>Canto</cite>,<cite>Pope</cite> | ||
It is important to complete the history with information about past history (prior history of ischemic events or vascular disease), risk factors for cardiovascular disease (o.a. smoking, hypertension, hyperlipidemia, obesity) and family history (direct family with myocardial infarction and/or sudden cardiac death). | It is important to complete the history with information about past history (prior history of ischemic events or vascular disease), risk factors for cardiovascular disease (o.a. smoking, hypertension, hyperlipidemia, obesity) and family history (direct family with myocardial infarction and/or sudden cardiac death). | ||
Signs of heart failure such as orthopnea (not able to sleep without a pillow), progressive dyspnoea and oedematous ankles are indicative for the extent of the problem. | Signs of heart failure such as orthopnea (not able to sleep without a pillow), progressive dyspnoea and oedematous ankles are indicative for the extent of the problem.<cite>Antman</cite> | ||
A suspected myocardial infarction should be rapidly evaluated to initiate appropriate therapy. | A suspected myocardial infarction should be rapidly evaluated to initiate appropriate therapy. | ||
==Physical Examination== | ==Physical Examination== | ||
On physical examination evidence of systemic hypoperfusion can be found such as hypotension, tachycardia, impaired cognition, pale and ashen skin. | On physical examination evidence of systemic hypoperfusion can be found such as hypotension, tachycardia, impaired cognition, pale and ashen skin.<cite>Antman</cite> | ||
If during auscultation pulmonary crackles are heard and pitting oedema of the ankles is seen heart failure is complicating the myocardial infarction. | If during auscultation pulmonary crackles are heard and pitting oedema of the ankles is seen heart failure is complicating the myocardial infarction. | ||
History and physical examination are helpful to determine myocardial infarction as diagnosis and to exclude other causes of chest pain, such as angina pectoris, aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems. PMID | History and physical examination are helpful to determine myocardial infarction as diagnosis and to exclude other causes of chest pain, such as angina pectoris, aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems.<cite>Antman</cite> | ||
==Electrocardiogram== | |||
An electrocardiogram (ECG) should be made within 10 minutes of arrival in every patient with suspected myocardial infarction.<cite>Antman</cite> | |||
An ECG is important to differentiate between myocardial ischemia and infarction: | |||
* ST elevation in myocardial infarction | |||
* ST depression in myocardial ischemia | |||
And to differentiate between STEMI and NSTEMI: | |||
* STEMI stands for ST elevated (>20 min) Myocardial Infarction | |||
* NSTEMI stand for Non ST elevated Myocardial Infarction | |||
It can however take 90 minutes after the onset of the symptoms to see abnormalities on the ECG. Therefore it is important to make a serial ECG, certainly if a patient has ongoing symptoms.<cite>Antman</cite> | |||
An ECG is also helpful in localising the ischemia: | |||
Anterior wall ischemia - One or more of leads V1-V6 | |||
Anteroseptal ischemia - Leads V1 to V3 | |||
Apical or lateral ischemia - Leads aVL and I, and leads V4 to V6 | |||
Inferior wall ischemia - Leads II, III, and aVF | |||
==Cardiac Markers== | |||
Cardiac markers are essential for confirming the diagnosis of infarction. Elevated CK MB and Troponin I indicate damage of the myocardium. Cardiac Troponin I concentration begins to rise two to three hours after myocardial ischemia.<cite>Macrae</cite> | |||
It can take 4-6 hours before the CK MB concentration is elevated. The advise is to repeat the measurements after 4-6 hours.<cite>Puleo</cite> | |||
A pitfall concerning elevated Troponin I can be patients with renal failure or pulmonary embolism.<cite>Thygesen</cite> Although cardiac markers are helpful for confirming the diagnosis reperfusion should not always wait till the cardiac markers are known. | |||
=ST elevated Myocardial Infarct= | |||
Initial treatment of STEMI is relief of ischemic pain, stabilize the hemodynamic status and reduce the ischemia as quickly as possible by fibrinolysis or primary percutaneous coronary intervention (PCI). Meanwhile other measures as continuous cardiac monitoring, oxygen and intravenous access are necessary to guarantee the safety of the patient.<cite>Antman</cite> | |||
Rapid revascularisation is essential to minimize the impact of the myocardial infarction and thereby reduce mortality. In the first hours after symptom onset the amount of salvageable myocardium by reperfusion is greatest. <cite>Anderson2</cite>, <cite>Bassand</cite> | |||
Revascularisation can be achieved by fibrinolysis or PCI. | |||
PCI is, if available, the preferred revascularisation method for patients with STEMI. | |||
But not all hospitals are qualified to perform PCI and therefore fibrinolysis is still used. There are however some circumstances in which transfer to a PCI qualified hospital is essential: | |||
• Patients with contraindications for fibrinolysis as active bleedings, recent dental surgery, past history of intracranial bleeding. PMID 14532318 | |||
• Patients with cardiogenic shock, severe heart failure and/or pulmonary oedema complicating the myocardial infarction. PMID 16186438, PMID 12472924 | |||
Or when PCI has a better outcome: | |||
• Patients who present three hours to four hours after the onset of the symptoms. PMID 12559937 | |||
• Patients with a non diagnostic ECG or a atypical history a coronary angiography with the ability to perform a PCI is preferred. PMID 12559937 | |||
FIBRINOLYSIS | |||
Fibrinolytics like streptokinase stimulate the conversion of plasminogen to plasmin. Plasmin demolishes fibrin which is an important constituent of the thrombus. Fibrinolytics are most effective the first hours after the onset of symptoms, after twelve hours the outcome will not improve.<cite>Bassand</cite> | |||
Because re occlusion after fibrinolysis is possible patients should be transferred to a PCI qualified hospital once fibrinolysis is done. PMID 15769784 | |||
PERCUTANEOUS CORONARY INTERVENTION (PCI) | |||
Table 3 Considerations for selecting primary percutaneous coronary intervention (PCI) for reperfusion therapy in patients with ST elevation myocardial infarction (STEMI) | |||
The procedure of PCI starts off as a coronary angiography (see CAG). When the stenosis is visualized a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is positioned at the site of the stenosis. To reduce the risk of coronary artery stent thrombosis antiplatelet therapy should be given. | |||
| Line 117: | Line 173: | ||
#Constant pmid=6831781 | #Constant pmid=6831781 | ||
#Anderson pmid=17692738 | #Anderson pmid=17692738 | ||
#Anderson2 pmid= | #Anderson2 pmid=8712096 | ||
#Abrams pmid=3925741 | #Abrams pmid=3925741 | ||
#Henrikson pmid=14678917 | #Henrikson pmid=14678917 | ||
#Antman pmid=15289388 | #Antman pmid=15289388 | ||
#Fox pmid=17162834 | #Fox pmid=17162834 | ||
#Amanullah pmid=1352191 | #Amanullah pmid=1352191 | ||
#Brown pmid=2007701 | #Brown pmid=2007701 | ||
| Line 132: | Line 186: | ||
#Hennekens pmid=9355934 | #Hennekens pmid=9355934 | ||
#Davies3 pmid=11084798 | #Davies3 pmid=11084798 | ||
#Swap pmid=16304077 | |||
#Macrae pmid=16556688 | |||
#Thygesen pmid=17951284 | |||
#Puleo pmid=7702648 | |||
#Bassand pmid=16311237 | |||
#Ref1 pmid=8375424 | #Ref1 pmid=8375424 | ||
</biblio> | </biblio> | ||
Revision as of 10:55, 10 August 2011
In 1772 doctor William Heberden first described angina pectoris, he wrote: “They who are afflicted with it are seized, while they are walking (more especially if it be up hill), with a painful and most disagreeable sensation in the breast, which seems as if it would extinguish life if it were to increase or to continue, but the moment the patient stands still all this uneasiness vanishes”.Davies
Three major coronary arteries provide the heart with oxygenated blood, the right coronary artery (RCA), the left coronary artery (LCA) and the circumflex artery (Cx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries narrows, the heart receives less oxygenated blood and becomes hypoxic, which results in angina pectoris.
Complete history and physical examination are essential to determine angina pectoris as diagnosis and to exclude other causes of chest pain, such as aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems.Sampson
History
Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back.Foreman Some patients only complain about stomach ache so the presentation can be very a specific.Canto,Pope
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately.Constant
Angina pectoris usually occurs during exercise when the demand for oxygenated blood increases. Coronary arteries with a narrowed lumen can not meet the demand of oxygenated blood during exercise. As soon as the exercise is aborted angina pectoris decreases. This is called stable angina pectoris.
Unstable angina pectoris means angina pectoris at rest which consists less than two months. Over time the angina pectoris develops to more often, severe and prolonged, so that symptoms are to occur at less and less effort than before.Anderson
Stable angina pectoris responds to nitro-glycerine spray, unstable angina pectoris does not. Nitro-glycerine spray is a venodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also vasodilates the coronary arteries and increases coronary blood flow.Abrams
Nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine also relaxes smooth muscle.Henrikson
During angina pectoris so called vegetative symptoms can occur, this includes sweating, nausea, paleface, anxiety and agitation. The idea is that the vegetative nerve system is more active in a reaction to stress.Antman
Physical Examination
Oxygen deficiency of the heart leads to ischemia, ischemia and the discomfort the patient experiences lead to sympathetic activation of the nervous system. This is detectable during physical examination by an increase in heart rate and elevation in blood pressure. Ischemia can also cause a temporarily impairment in myocardial function, on auscultation you could hear a paradoxically split second heart sound, a third or fourth heart sound and a mitral regurgitation murmur. All these findings however disappear with resolution of the ischemia. Up to date: Pathophysiology and clinical presentation of ischemic chest pain, geen bronvermelding.
ECG
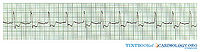
The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression. Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities.Ref1 During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities.Fox
Additional Research
If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done.Fox Depending on the hospital one of the below standing research will be done.
- Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity.Amanullah
- Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest.Brown
- MRI can be done with vasodilatory dobutamine or stimulating adenosine to assess how the heart behaves during exercise.Kwong
The findings on stress testing can be used to determine the choice between medical therapy and revascularization in patients with stable angina. Coronary angiography is recommended based upon symptoms, left ventricular function, and estimated risk by stress testing.Fraker
Table 1
Coronary Angiography
In patients with unstable angina pectoris early coronary angiography possibly followed by revascularization is usually performed within 4 to 24 hours of admission in the hospital. In most clinical trials this strategy has shown a reduction in the incidence of death or nonfatal myocardial infraction.Anderson
A CAG is an X ray examination of the coronary arteries, a catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. Contrast is visible by X ray and the images that are obtained are called angiograms.
On an angiogram stenoses will be visible, if the stenosis is significant coronary intervention will take place. Ideally this happens immediately following the CAG but not all hospitals that are entitled to carry out CAG are qualified to perform percutaneous coronary intervention (PCI).
Treatment
Medication
In patients with stable angina pectoris percutaneous coronary intervention does not offer any benefit in terms of death, myocardial infarction, or the need for subsequent revascularization compared with conservative medical treatment.Katritsis
Initial treatment of stable angina pectoris therefore focuses on medication to keep the workload of the heart as low as possible. β blockers lower heart rate and blood pressure, this decreases the oxygen demand of the heart.Garcia Nitrates dilatate the coronary arteries so the heart receives more oxygenated blood.Abrams Anticoagulants (aspirin) to reduce the risk of development of a thrombus in the coronary arteries.Hennekens
Apart from starting medication the patient needs to minimize any present risk factors like smoking, overweight and drinking alcohol. See chronic coronary diseases.
Percutaneous Coronary Intervention
The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is often positioned at the site of the stenosis.
Coronary Artery Bypass Graft
There are circumstances in which CABG should be performed.
| Class of recommendations | Definition |
|---|---|
| Class I | Evidence and/or general agreement that a given treatment or procedure is beneficial, useful, effective. |
| Class II | Conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of the given treatment or procedure.
|
| Class III | Evidence or general agreement that the given treatment or procedure is not usefull effective, and in some cases may be harmful. |
| Class I - There is evidence and/or general agreement that CABG should be performed in patients with STEMI in the following settings. | |
CABG does not eliminate the stenosis like PCI does. Using the internal thoracic arteries or the saphenous veins from the legs a bypass is made around the stenosis. The bypass originates from the aorta and terminates directly after the stenosis. Thereby restoring the blood supply to the ramifications.
Myocardial Infarction
In 2006 425.425 people died from a heart attack, 1.255.000 new and recurrent coronary attacks took place, about 34% died, 17.600.000 victims of angina, heart attack and other forms of coronary heart disease are still living.
These numbers only account for the United States.
Pathofysiology
A heart attack or myocardial infarction (MI) is an acute presentation of a process that has been going on much longer. The process responsible is atherosclerosis. Atherosclerosis is a chronic disease of the arteries in which artery walls thicken by deposition of fatty materials such as cholesterol. The result over decades are plaques, which can narrow the lumen of the arteries significantly and progressively causing symptoms as angina pectoris. Plaques can also suddenly rupture, trigger a cascade which results in a thrombus and thereby cause myocardial infarction.Davies3
History
Classic presentation of a myocardial infarction is acute chest pain which lasts longer than a few minutes.Swap The pain does not decrease at rest and is only temporarily relieved with nitroglycerin. Common accompanying symptoms are radiating pain to shoulder, arm, back and/or jaw.Foreman Shortness of breath can occur, as well as sweating, fainting, nausea and vomiting, so called vegetative symptoms. Some patients not really complain about chest pain but more about abdominal pain so as with angina pectoris the presentation can be very a specific.Canto,Pope
It is important to complete the history with information about past history (prior history of ischemic events or vascular disease), risk factors for cardiovascular disease (o.a. smoking, hypertension, hyperlipidemia, obesity) and family history (direct family with myocardial infarction and/or sudden cardiac death).
Signs of heart failure such as orthopnea (not able to sleep without a pillow), progressive dyspnoea and oedematous ankles are indicative for the extent of the problem.Antman
A suspected myocardial infarction should be rapidly evaluated to initiate appropriate therapy.
Physical Examination
On physical examination evidence of systemic hypoperfusion can be found such as hypotension, tachycardia, impaired cognition, pale and ashen skin.Antman
If during auscultation pulmonary crackles are heard and pitting oedema of the ankles is seen heart failure is complicating the myocardial infarction.
History and physical examination are helpful to determine myocardial infarction as diagnosis and to exclude other causes of chest pain, such as angina pectoris, aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems.Antman
Electrocardiogram
An electrocardiogram (ECG) should be made within 10 minutes of arrival in every patient with suspected myocardial infarction.Antman An ECG is important to differentiate between myocardial ischemia and infarction:
- ST elevation in myocardial infarction
- ST depression in myocardial ischemia
And to differentiate between STEMI and NSTEMI:
- STEMI stands for ST elevated (>20 min) Myocardial Infarction
- NSTEMI stand for Non ST elevated Myocardial Infarction
It can however take 90 minutes after the onset of the symptoms to see abnormalities on the ECG. Therefore it is important to make a serial ECG, certainly if a patient has ongoing symptoms.Antman
An ECG is also helpful in localising the ischemia: Anterior wall ischemia - One or more of leads V1-V6 Anteroseptal ischemia - Leads V1 to V3 Apical or lateral ischemia - Leads aVL and I, and leads V4 to V6 Inferior wall ischemia - Leads II, III, and aVF
Cardiac Markers
Cardiac markers are essential for confirming the diagnosis of infarction. Elevated CK MB and Troponin I indicate damage of the myocardium. Cardiac Troponin I concentration begins to rise two to three hours after myocardial ischemia.Macrae It can take 4-6 hours before the CK MB concentration is elevated. The advise is to repeat the measurements after 4-6 hours.Puleo A pitfall concerning elevated Troponin I can be patients with renal failure or pulmonary embolism.Thygesen Although cardiac markers are helpful for confirming the diagnosis reperfusion should not always wait till the cardiac markers are known.
ST elevated Myocardial Infarct
Initial treatment of STEMI is relief of ischemic pain, stabilize the hemodynamic status and reduce the ischemia as quickly as possible by fibrinolysis or primary percutaneous coronary intervention (PCI). Meanwhile other measures as continuous cardiac monitoring, oxygen and intravenous access are necessary to guarantee the safety of the patient.Antman
Rapid revascularisation is essential to minimize the impact of the myocardial infarction and thereby reduce mortality. In the first hours after symptom onset the amount of salvageable myocardium by reperfusion is greatest. Anderson2, Bassand Revascularisation can be achieved by fibrinolysis or PCI.
PCI is, if available, the preferred revascularisation method for patients with STEMI. But not all hospitals are qualified to perform PCI and therefore fibrinolysis is still used. There are however some circumstances in which transfer to a PCI qualified hospital is essential:
• Patients with contraindications for fibrinolysis as active bleedings, recent dental surgery, past history of intracranial bleeding. PMID 14532318 • Patients with cardiogenic shock, severe heart failure and/or pulmonary oedema complicating the myocardial infarction. PMID 16186438, PMID 12472924
Or when PCI has a better outcome:
• Patients who present three hours to four hours after the onset of the symptoms. PMID 12559937 • Patients with a non diagnostic ECG or a atypical history a coronary angiography with the ability to perform a PCI is preferred. PMID 12559937
FIBRINOLYSIS Fibrinolytics like streptokinase stimulate the conversion of plasminogen to plasmin. Plasmin demolishes fibrin which is an important constituent of the thrombus. Fibrinolytics are most effective the first hours after the onset of symptoms, after twelve hours the outcome will not improve.Bassand Because re occlusion after fibrinolysis is possible patients should be transferred to a PCI qualified hospital once fibrinolysis is done. PMID 15769784
PERCUTANEOUS CORONARY INTERVENTION (PCI)
Table 3 Considerations for selecting primary percutaneous coronary intervention (PCI) for reperfusion therapy in patients with ST elevation myocardial infarction (STEMI)
The procedure of PCI starts off as a coronary angiography (see CAG). When the stenosis is visualized a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is positioned at the site of the stenosis. To reduce the risk of coronary artery stent thrombosis antiplatelet therapy should be given.
References
<biblio>
- Davies pmid=11756201
- Sampson pmid=4997794
- Foreman pmid=10099685
- Canto pmid=10866870
- Pope pmid=10751787
- Constant pmid=6831781
- Anderson pmid=17692738
- Anderson2 pmid=8712096
- Abrams pmid=3925741
- Henrikson pmid=14678917
- Antman pmid=15289388
- Fox pmid=17162834
- Amanullah pmid=1352191
- Brown pmid=2007701
- Kwong pmid=12566362
- Fraker pmid=18061078
- Katritsis pmid=15927966
- Garcia pmid=16735367
- Hennekens pmid=9355934
- Davies3 pmid=11084798
- Swap pmid=16304077
- Macrae pmid=16556688
- Thygesen pmid=17951284
- Puleo pmid=7702648
- Bassand pmid=16311237
- Ref1 pmid=8375424
</biblio>