Tachycardia
Content is incomplete and may be incorrect. |
Sébastien Krul, MD, Louise Olde Nordkamp, MD, Jonas de Jong, MD
Introduction
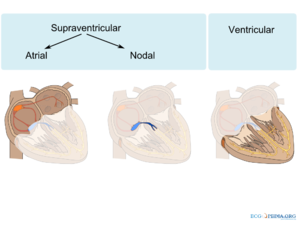
Differentiation between supraventricular tachycardias (SVT) and ventricular tachycardias (VT) can be challenging, especially in acute emergency settings. SVT's are arrhythmias in the atria or AV-node or arrhythmias in which these structures are involved. Supraventricular arrhythmias are relatively common and rarely life-threatening. VT's are rhythm disorders that origin from the ventricles. VTs can both take place in the myocardial tissue and the conduction system tissue (Figure 1).
Supra-ventricular tachycardia
Atrial arrhythmias
The following arrhythmias arise in the atrium. Dependent on the refractory period of the AV-node the ventricles follow the atrial activation at the same rate at higher atrial rates the AV-node starts to block conduction from atrium to ventricle.[2][3]
Sinus Tachycardia
Pathophysiology:
When the sinus node fires with a frequency rate between 100-180bpm, the term sinustachycardia is used. The maximum heart rate a person can achieve during exercise can be calculatedbe estimated by subtracting the age in years from 210, although it is not uncommon for sinus rates to peak above 200/min during vigorous exercise. Usually it is a physiological reaction to stress (exercise, inflammation, stress). External factors can increase the heart rate like coffee and alcohol or drugs.[4] The term inappropriate sinus tachycardia is a persistent increase in resting heart rate or sinus rate unrelated to or an exaggerated response to stress in a person without structural heart disease.[5]
Clinical diagnosis:
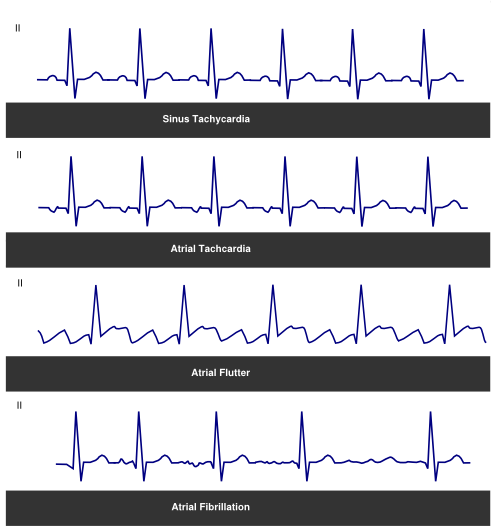
A sinus tachycardia usually has a gradual start and ending. Diagnosis on the ECG can be made by the morphology of the P-wave. The P-wave has the same morphology during sinus tachycardia as during normal sinus rhythm (Figure 2).[6][7] An inappropriate sinus tachycardia is diagnosed by when the sinus tachycardia is persistent (therefore non-paroxysmal) and no trigger can be identified.
Management:
No treatment is indicated; usually the sinustachycardia will pass when the external trigger is removed. If patients have persistent complaints, the trigger cannot be removed or in case of an inappropriate sinus tachycardia a beta-blocker can be administered. Patients with a contra-indication for beta-blockers can use nondihydropyridine calcium-channel blockers.
Atrial Tachycardia (AT)
Pathophysiology:
Atrial tachycardia (AT) is a tachycardia resulting from fast firing in an ectopic focus or micro re-entry circuit in the atria.[8] It has a rate of ≥ 100bpm. In some patients the tachycardia has multiple foci (multifocal atrial tachycardia). This results in different P-wave morphologies on the ECG during the arrhythmia. Atrial tachycardia can be caused by all the mechanisms of arrhythmia formation. Patients after earlier surgery or catheter ablation usually present with macro re-entry AT located around functional or anatomical sides of block. Atrial flutter is a distinct type of AT, but due to its unique mechanism it is discussed separately.
Clinical diagnosis:
ATs have a wide range clinical presentation. They can occur in paroxysms or can be the permanent underlying rhythm. Complaints of palpitation and a fast regular heart rate are common and as a result of the tachycardia complaints of dizziness, dyspnoea and syncope can be experienced. Focal AT that with a progressive increase at onset and decrease before termination are likely based on abnormal automaticity. Digoxine intoxication is a common cause for ATs. On the ECG an atrial tachycardia can be detected through the P-wave morphology. The P-wave has a different morphology depending on the foci of the atrial tachycardia (Figure 2). An ECG in resting condition of sinus rhythm can help distinguish different morphologies and help in localization of the source of the atrial tachycardia. Vagal manoeuvres or administration of adenosine can block the AV-conduction and reveal firing from the atrium, thereby clearly identifying the atrial source of the tachycardia. Some ATs are sensitive to adenosine and will terminate after administration of adenosine. However sometimes only an electrophysiological study can differentiate between the different SVT and localize the precise location or circuit of the AT.[6][7][9]
Management:
Vagal manoeuvres or adenosine can be effective in terminating focal AT.[10] If AT persist and is drug-resistant DC cardioversion can be indicated. Recurrent episodes of AT can be prevented with anti-arrhythmic medication, for instance with beta-blockers or calcium antagonists. However not all AT are sensitive to medication and success rate of medication is usually low. If these drugs are unsuccessful Class IC in combination with AV-nodal-blocking agents or Class III drugs can be tried.[11] The treatment of choice for symptomatic AT is catheter ablation. In an experienced centre up to 90% of the ATs can be ablated, recurrence rate is relatively high often due to a new focus of AT. Treatment of multifocal atrial tachyardia is difficult and therapy is usually directed at the management of underlying disease.[12][13]
Atrial Flutter (AFL)
Pathophysiology:
Atrial flutter (AFL) is the most common type of atrial tachycardia. The typical AFL is dependent of the cavotricuspid isthmus.[8] The isthmus between the caval vein and tricuspid is an area of slow conduction. Due to this slow conduction counter clockwise re-entry around the tricuspid annulus can exist. This re-entry produces a typical arrhythmia with activates the atria at a rate between 250-350 beats per minute. If the re-entry circuit moves counter clockwise a typical AFL is produced. If the re-entry circuit moves clockwise, a atypical AFL is seen.[14] The causes and risk are comparable with atrial fibrillation.
Clinical diagnosis:
An AFL is usually paroxysmal, with a sudden onset, and is diagnosed on the ECG by it typical saw tooth pattern. Patients experience complaints of palpitations, dyspnoea, fatigue or chest pain. An AFL typically has an atrial rate of 280-320 bpm, which conducts to the ventricles in 2:1, 3:1 or 4:1 manner. The P-wave morphology has a saw tooth like appearance and in a typical AFL has a negative vector in the inferior leads. The upstroke or down stroke of the first part of the P-wave is fast, the second path slow (Figure 2). In an atypical AFL the inferior leads have a positive vector. Atrial fibrillation is a common finding in patients with an AFL (up to 35%).[6][7][9][15]
Management:
A patient with an acute episode of AFL requires cardioversion. This can be achieved with anti-arrhythmic drugs or electrical cardioversion. Vagal manoeuvres increase the AV-block on the ECG and demonstrate the AFL more clearly. Anti-arrhythmic drugs are modestly effective in the acute setting (ibutilide or dofetilide) and, but have the risk of pro-arrhythmic effects.[16][17][18] DC cardioversion is an effective methods to cardiovert AFL, especially in patients with heart failure or hemodynamic instability. AFL is amendable to catheter ablation and this is the treatment of choice in AFL. Targeted ablation of the area between the inferior vena cava and the tricuspid annulus can block the re-entry circuit. This is a very successful procedure, with few complications in the hands of an experienced electrophysiologist.[19][20][21] If patients are not eligible for ablation, anti-arrhythmic drugs class IC or III can be started. However they are of limited efficacy and class IC drugs not be administered without AV-nodal slowing agent because of atrial slowing can result in 1:1 AV conduction. Patients with AFL require anti-coagulation as in atrial fibrillation according to the CHADSVASc score.[22][23]
Atrial Fibrillation (AF)
Pathophysiology:
The pathophysiology of AF is complex and incompletely understood.[24] In most patients the trigger of AF results from extra beats in from the pulmonary veins.[25] This is due to myocardial sleeves growing into the pulmonary veins, which are triggered to fire extra beats due a variety of modulators (i.e. the autonomic nerve system).[26] These triggers can trigger the atria into forming multiple self-perpetuating re-entry circuits. These multiple wavelets, are self-perpetuating circuits than constantly change and move through the atria. The ability of the atria to sustain AF is dependable on atrial structural changes (fibrosis/inflammation). AF induces electromechanical changes in the atrium. These changes make it easier for AF to perpetuate; AF begets AF.[27] Due to the fast and rapid activation of the atria, there is no functional mechanical activity left. This results in the most feared complication of AF, namely forming of blood clots (with for instance stroke as a result). During atrial standstill the atria does not effectively pump blood to the ventricle, and blood can coagulate the left atrium or left atrial appendage.[28] The strokes resulting from AF are often more severe than other causes of stroke. Another complication of AF is a tachycardiomyopathy. Due to the constant chaotic activity in the atria, the AV-node can conduct these signals at high rate. The result is an irregular fast ventricular activation. These fast activation of the ventricle can lead to a (reversible) dilated cardiomyopathy.[29]
| Classification of Atrial Fibrillation (AF) related symptoms based on the European Heart Rhythm Association (EHRA) score are: [30] | |
| EHRA I | No symptoms |
|---|---|
| EHRA II | Mild symptoms; normal daily activity not affected |
| EHRA III | Severe symptoms; normal daily activity affected |
| EHRA IV | Disabling symptom; normal daily activity discontinued |
Clinical diagnosis:
AF is the most common supraventricular arrhythmia in Western society. Patients can experience complaints from palpitations, dyspnoea and dizziness. Prevalence increases with age and reaches 7-10% in 80 year olds. It is characterized by the absence of clear P-waves on the surface ECG and an irregular ventricular rate (Figure 2). On physical examination an irregular pulse can be felt, however this is not diagnostic of AF as other causes can cause an irregular pulse (mainly atrial or ventricular extra systoles). The cardiac output is 10% reduced due to lack of atrial kick. Furthermore due to the higher ventricular rate the heart has not enough time to completely fill with blood thereby reducing stroke volume. The development of AF is associated with different diseases, e.g. hypertension, mitral valve disease, thyroid disease and diabetes.[31] AF usually starts with short single isolated episodes of AF which are self terminating. Progressively over time these episodes are of longer duration and occur more frequently. These episodes progress to persistent AF, which is defined as AF lasting longer than 7 days or which can only be terminated by cardioversion. In the end AF is permanent and cardioversion is not possible or duration of sinus rhythm is short.[32] Episodes of AF can be symptomatic, but patients can experience no symptoms during AF. However it is important to note that the risks of complications of AF are unrelated to the duration of the episodes.[33] AF is classified according to the clinical presentation of AF:[34]
- Paroxysmal atrial fibrillation: Episodes AF lasting shorter than 7 days and terminating spontaneously usually within 48 hours.
- Persistent atrial fibrillation: Episodes of AF not terminating spontaneously or lasting longer than 7 days or requires cardioversion
- Long standing persistent atrial fibrillation: Persistent AF for more than one year.
- Permanent atrial fibrillation: Accepted AF, no strategies of rhythm control are pursued.
Management:
| Acute Management: |
|---|
The acute management of AF depends on the presentation of the patient. In stable patients with little complaints, rate control can be initiated with beta-blockers, non-dihydropyridine Ca-antagonists and digoxine. If the patient has recent onset of AF, is highly symptomatic or hemodynamicly compromised, cardioversion is indicated. Cardioversion can be performed medically or with electricity. The most effective drug for chemical cardioversion is flecainide, although this drug is contra-indicated in patients with structural heart disease or ischemia.[35] Another option is ibutilide, but this is mostly used and more effective to terminate AFL, and has a small risk of ventricular arrhythmias.[18] In patients with severe structural heart disease amiodarone can be given.[36] Electrical cardioversion can achieved by a DC shock after sedation of the patient. If the AF persist for longer than >48 hours or the start of the episode is not clear, anti-coagulation should be initiated before (medical or electrical) cardioversion. Three weeks of adequate anti-coagulation is advised before cardioversion and it should be continued after cardioversion for 4 weeks to minimize thromboembolic risk.
| Long-Term Management: |
|---|
The management of AF consists of several key targets. Firstly, any underlying potential reversible cause of AF should be treated. Secondly, care should be taken to prevent the complications of AF. This means that adequate oral-anticoagulation should be initiated and rate control should be started to reduce heart rate. Thirdly, symptoms should be treated with medical or invasive therapy. There are two strategies to reduce symptoms of AF. Rate control is a strategy where a reduction of ventricular heart rate is the main goal. In rhythm control the aim is to maintain sinus rhythm and prevent recurrences of AF.[34] [37]
| Rate control: |
In AF the ventricle can have a fast irregular rate that can lead to complaints of palpitations and a tachycardiomyopathy. One of the strategies in managing AF is to control ventricular rate <110bpm.[38][39] In patients with persistent complaints or with heart failure a resting heart rate of <80 is advised. In this strategy no attempt is made to achieve sinus rhythm. This is the only treatment option in patients with permanent AF. Due to the fast irregular ventricular rate a dilated tachycardiomyopathy can develop and proper rate control can revert these ventricular changes. Rate control can be achieved with beta-blockers or non-dihydropyridine Ca-antagonists. Digoxine can be added to rate control, however a recent study showed an increase in mortality in patients using digoxine.[40] If rate control cannot be achieved with drugs, His ablation after pacemaker implant is indicated.
- His-Ablation with pacemaker implantation:
Patients with accepted AF and complaints of a high irregular ventricular rate who do not tolerate medication can be helped with a targeted His bundle ablation with catheter ablation to induce complete AV-block. Before His ablation a pacemaker should be implanted to assure an adequate ventricular rate and response to exercise.
| Rhythm control: |
In rhythm control all efforts are made to achieve and maintain sinus rhythm. This can be done with anti-arrhythmic drugs. Most effective are the Class IC and III anti-arrhythmic drugs.[41] Overall rhythm control is difficult and anti-arrhythmic drugs might have (pro-arrhythmic) side effects, if patients have contra-indications.[42][43] Therefore prescription of these drugs should occur with caution. If patients experience serious side effects of anti-arrhythmic drugs or have a low frequency of AF episodes a one month treatment with anti-arrhythmic drugs (especially flecainide combined with beta blocker or non-dihydropiridine calcium antagonist) after cardioversion can prevent the majority of recurrences.[44] Amiodarone is unsuitable for short-term treatment due to its pharmacological properties.[45]
| Invasive treatment:[46] |
|---|
| Catheter ablation: |
Medical therapy is not always sufficient to maintain sinus rhythm. In the last decade of 20th century it was discovered that AF is triggered from the pulmonary veins and that selective ablation of these trigger sites can reduce AF recurrence.[47] As this technique evolved it is now common to ablate an area around the pulmonary veins to isolate them from the atrial tissue. The left atrium is approached through the inter-atrial septum and with the use of imaging and electrocardiographic signals a 3D map is made to navigate the atria. The pulmonary vein isolation can be performed with multiple energy sources (cryo-cooling, radiofrequent energy). This is a complex procedure that depending on the technique used has a minor chance of (severe) complications (1-5%), primarily caused by damage of the surrounding structures. The one year success rate of the procedure varies on the experience of the operator and is a freedom of AF in 57-71% of the patients after one or more procedures.[48][49] Catheter ablation is suitable for patients with a with drug-refratory rhythm control strategy.[50] Certain selected patients with heart failure might benefit from catheter ablation, although success is lower.[51][52]
| Surgical treatment: |
Surgery is a more invasive, but effective modality to treat AF. The classical cut and sew Maze procedure is an open chest procedure that requires extra-corporeal circulation. In this procedure the atrium is cut and sewn again to compartmentalize the atrium en therefore prevent the atrium maintaining AF.[53][54] In recent years a less invasive procedure has developed to treat AF. This minimal invasive surgery is performed through thoracotomy or thoracoscopy and is performed on a beating heart.[55] A pulmonary vein isolation is performed with a clamp and if patients have persistent AF additional left atrial lesions are made on the atrium to compartmentalize the atrium. Finally the left atrial appendage is removed to reduce the occurrence of stroke. This procedure has a success rate of 68% after one year.[56][57][58] Recently hybrid surgical procedures have been described that combine the minimal invasive thoracoscopic surgery with (epicardial or endocardial) elektrophysiological measurement. Patients with a large left atrium (diameter>45mm) or a failed catheter ablation are eligible for AF surgery.[59][60]
Studies have shown no benefit of rhythm control over rate control, thus the selection of strategy is mainly dependent of patient and AF characteristics.[38][61][62][63][64][65][66] Patients with AF and heart failure have limited medical options of rate control, as most anti-arrhythmic drugs are contra-indicated, and no benefit of rate vs. rhythm control was detected in studies.[67][68] This means that, since rate control is easier to achieve, rate control should be the initial strategy in all patients, especially in old patients and patients with no or few symptoms of AF. The target heart rate to achieve in rest is <110 beats per minute.[69] In patients with persistent complaints of AF rhythm control can be initiated on top of rate control. Young patients with paroxysmal AF and no underlying heart disease might benefit from early (invasive) rhythm control to halt progression of the disease.[70] However, independent of the treatment strategy, proper anti-coagulation is important and necessary in patients with risk factors.[34][37]
| CHA2DS2VASc score to estimate stroke risk | ||
|---|---|---|
| Risk Factor | Points | |
| C: | Congestive heart failure | 1 point |
| H: | Hypertension | 1 point |
| A: | Age>75years | 2 point |
| D: | Diabetes | 1 point |
| S: | Stroke/Embolism | 2 points |
| V: | Vascular Disease | 1 point |
| A: | Age>65years | 1 point |
| Sc: | Female Sex | 1 point |
| Anticoagluation treatment: |
Proper anti-coagulation is important in patients with AF to reduce the occurrence of stroke.[28] In patients with AF the indication of anti-coagulation is based on certain patient-related risk-factors. A score is created to facilitate the clinical decision making. The CHADS2VASc2 score incorporates these risk factors. A patient has no indication for anti-coagulation if there is a low-risk of thromboembolic complications.[71][72] These patients are defined as males or females <65 years old with no other risk factors. This translates ins a CHADSVASc score of 0, or a CHADSVASc score of 1, where 1 point is based on the female sex. In all other cases anti-coagulation with coumarins or other new anticoagulation drugs (dabigatran, rivaroxiban, apixaban)[73][74][75] is indicated if no strong bleeding-risk exist. It is important to note that anti-coagulation is independent of the underlying rhythm.
AV-nodal arrhythmias
This section covers the arrhythmias in which the AV-node is critical in maintaining the arrhythmia. Most of these arrhythmias share the common characteristic that AV-node blocking or delaying manoeuvres or medication (adenosine) can terminate the arrhythmia.[2][3]
AV junctional tachycardia
An AV junctional tachycardia is a tachycardia resulting from regular frequent firing (110-250 bpm) of the AV-node. It has the characteristics of a small QRS with a retrograde or no P-wave. The P-wave is not always visible because it can be hidden in the QRS complex. If it is visible it is negative in the inferior leads and narrow, suggesting an AV-nodal origin. The small QRS is not preceded by a p-wave as atrium and ventricle are both activated from the AV-node. For management of this arrhythmia variable success is achieved with anti-arrhythmic drugs.
Atrioventricular Nodal Reciprocating Tachycardia (AVNRT)
Pathophysiology:
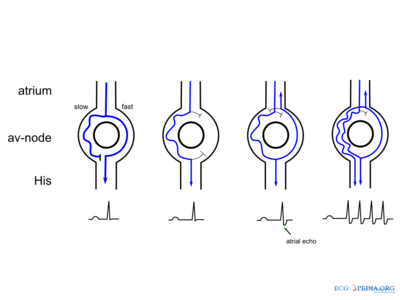
AVNRT is a regular arrhythmia relying on the dual AV-physiology for its maintenance. The AV-node usually has two pathways in these patients; a fast pathway with fast conduction times and a slow pathway, which conducts slowly. The fast pathway has a longer refractory period than the slow pathway. Due to these characteristics re-entry formation is possible. Normally the impulse from the atria is conducted through the fast pathway to the ventricle. The impulse also travels through the slow pathway, but reaches tissue still in the refractory period at the end of the AV-node (as the fast pathway has already conducted the impulse and activated this part of the AV-node). When an extra premature atrial contraction occurs it encounters a refractory fast-pathway (which has a longer refractory period). It enters the slow pathway and when it reaches the end of this pathway it can conduct to the (now restored) end of the AV-node to the ventricles