SQTS: Difference between revisions
mNo edit summary |
|||
| (4 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
<i>Auteur: Louise R.A. Olde Nordkamp</i> | <i>Auteur: Louise R.A. Olde Nordkamp</i> | ||
<i>Supervisor: Arthur A.M. Wilde</i> | <i>Supervisor: Arthur A.M. Wilde</i> | ||
| Line 5: | Line 6: | ||
==Clinical diagnosis== | ==Clinical diagnosis== | ||
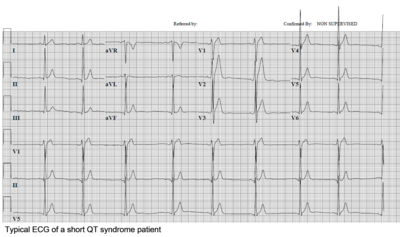
[[Image:ShortQT_syndrome_patient.png|thumb|right]] | [[Image:ShortQT_syndrome_patient.png|400px|thumb|right]] | ||
The diagnosis is based on the presence a short QT interval, in which the upper limit is mostly set on 330 ms. Males are more often affected than women. A history of cardiac arrest is present in one-third. Patients are at risk for both atrial arrhythmias (AF) and ventricular arrhythmias (VT/VF). | The diagnosis is based on the presence a short QT interval, in which the upper limit is mostly set on 330 ms. Males are more often affected than women. A history of cardiac arrest is present in one-third. Patients are at risk for both atrial arrhythmias (AF) and ventricular arrhythmias (VT/VF). | ||
| Line 18: | Line 19: | ||
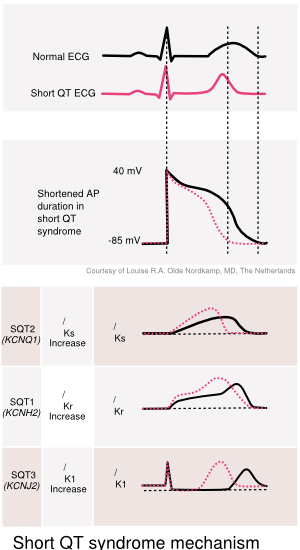
==Genetic diagnosis== | ==Genetic diagnosis== | ||
[[Image:ShortQT_syndrome_mechanism. | [[Image:ShortQT_syndrome_mechanism.svg|thumb|right]] | ||
In a quarter of the patients a mutation is found, predominantly in the KCNH2 gene (SQTS1). This gain-of-function mutation causes an increase in the potassium efflux and, subsequently, to a decrease of the myocyte refractory period. Mutations in the KCNQ1, KCNJ2 and possibly CACNxxx genes are also associated with the SQTS. | In a quarter of the patients a mutation is found, predominantly in the KCNH2 gene (SQTS1). This gain-of-function mutation causes an increase in the potassium efflux and, subsequently, to a decrease of the myocyte refractory period. Mutations in the KCNQ1, KCNJ2 and possibly CACNxxx genes are also associated with the SQTS. | ||
Latest revision as of 07:34, 26 March 2013
Auteur: Louise R.A. Olde Nordkamp
Supervisor: Arthur A.M. Wilde
The short QT syndrome is a very rare syndrome characterized by an abnormally short QT interval and increased risk of ventricular fibrillation and cardiac death.
Clinical diagnosis
The diagnosis is based on the presence a short QT interval, in which the upper limit is mostly set on 330 ms. Males are more often affected than women. A history of cardiac arrest is present in one-third. Patients are at risk for both atrial arrhythmias (AF) and ventricular arrhythmias (VT/VF).
Physical examination
Patients can present with symptoms of arrhythmias:
- Out-of-hospital-cardiac-arrest
- Syncope, pre-syncope (weakness, lightheadedness, dizziness)
ECG tests
The ECG demonstrates a corrected QT interval significantly below the limit of normal (<330 ms). Additionally, notable ECG findings are the presence of a sharp T-wave beginning at the end of the QRS complex, preceded by a brief or absent ST-segment. Exercise electrocardiographic studies in SQTS patients also characteristically reveal a non-physiologic lack of QT shortening at increased heart rates.
Genetic diagnosis
In a quarter of the patients a mutation is found, predominantly in the KCNH2 gene (SQTS1). This gain-of-function mutation causes an increase in the potassium efflux and, subsequently, to a decrease of the myocyte refractory period. Mutations in the KCNQ1, KCNJ2 and possibly CACNxxx genes are also associated with the SQTS.
Risk Stratification
Risk stratification in SQTS is still ill-defined and should be done by a specialized cardio-genetic cardiologist.
Treatment
Hydroquinidine is suggested for normalization of the QT interval in patients with a KCNH2 mutation. ICD therapy is advised in SQTS patients for secondary prevention of sudden cardiac death and could be considered
References
- Giustetto C, Di Monte F, Wolpert C, Borggrefe M, Schimpf R, Sbragia P, Leone G, Maury P, Anttonen O, Haissaguerre M, and Gaita F. Short QT syndrome: clinical findings and diagnostic-therapeutic implications. Eur Heart J. 2006 Oct;27(20):2440-7. DOI:10.1093/eurheartj/ehl185 |
- Giustetto C, Schimpf R, Mazzanti A, Scrocco C, Maury P, Anttonen O, Probst V, Blanc JJ, Sbragia P, Dalmasso P, Borggrefe M, and Gaita F. Long-term follow-up of patients with short QT syndrome. J Am Coll Cardiol. 2011 Aug 2;58(6):587-95. DOI:10.1016/j.jacc.2011.03.038 |
- Patel C, Yan GX, and Antzelevitch C. Short QT syndrome: from bench to bedside. Circ Arrhythm Electrophysiol. 2010 Aug;3(4):401-8. DOI:10.1161/CIRCEP.109.921056 |