Chest Pain / Angina Pectoris: Difference between revisions
No edit summary |
|||
| (79 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
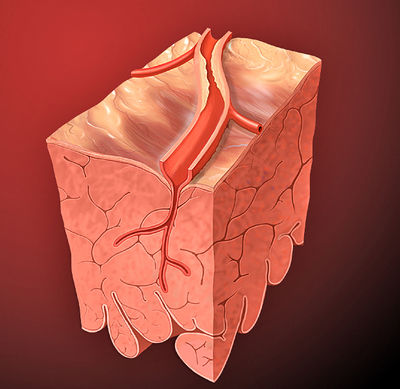
[[File:Heart_coronary_artery.jpg|thumb|400px|An epicardial coronary artery with a atherosclerotic narrowing]] | |||
Stable angina (pectoris) is a clinical syndrome characterized by discomfort in the chest, jaw, shoulder, back, or arms, typically elicited by exertion or emotional stress and relieved | |||
by rest or nitroglycerin. It can be attributed to myocardial ischemia which is most commonly caused by atherosclerotic coronary artery disease or aortic valve stenosis. | |||
Three major coronary arteries | Three major coronary arteries supply the heart with oxygenated blood, the right coronary artery (RCA), the left anterior descending coronary artery (LAD) and the left circumflex artery (LCx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries progressively narrow, a dysbalance between myocardial oxygen supply and myocardial oxygen consumption may occur, causing myocardial ischemia. | ||
In stable angina this imbalance mainly occurs when oxygen demand increases due to exercise, increased heart rate, contractility or wall stress. | |||
A complete history and physical examination are essential to support the diagnosis (stable) angina pectoris and to exclude other (acute) causes of chest pain such as an acute coronary syndrome, aortic dissection, arrhythmias, pulmonary embolism, (tension) pneumothorax or pneumonia, gastroesophageal reflux or spams, hyperventilation or musculoskeletal pain. <Cite>REFNAME2</Cite> In addition, laboratory tests and specific cardiac investigations are often necessary. | |||
==History== | |||
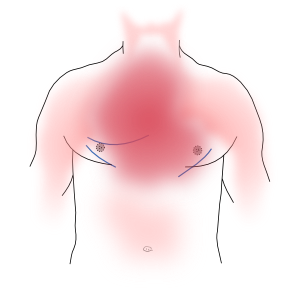
Patients often | [[File:Chest_pain_areas.svg|thumb|Typical chest pain is retrosternal. Pain may radiate to the arms, jaw, and / or back.]] | ||
Patients often describe angina pectoris as pressure, tightness, or heaviness located centrally in the chest, and sometimes as strangling, constricting, or burning. The pain often radiates elsewhere in the upper body, mainly arms, jaw and/or back. <Cite>REFNAME3</Cite> Some patients only complain about abdominal pain so the presentation can be aspecific. <Cite>REFNAME4</Cite>, <Cite>REFNAME5</Cite> | |||
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain | Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is usually is brief and gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain does not change with respiration or position. If patients had angina pectoris previously they are often able to recognize the pain immediately. <Cite>REFNAME6</Cite> | ||
Angina pectoris is a manifestation of arterial insufficiency and usually occurs with increasing oxygen demand such as during exercise. As soon as the demand is decreased (by stopping the exercise for example) complaints usually disappears within a few minutes. | |||
Another way to relieve pain is by administration of nitro-glycerine. Nitro-glycerine spray is a vasodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also dilates the coronary arteries and increases coronary blood flow. <Cite>REFNAME7</Cite> The response to nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine relaxes smooth muscle tissue. <Cite>REFNAME8</Cite> | |||
Depending on the characteristics, chest pain can be identified as typical angina, atypical angina or non-cardiac chest pain, see Table 1. | |||
{| class="wikitable" border="1" width="600px" | |||
|- | |||
! align="center" colspan="2" | Table 1. Clinical classification of chest pain <Cite>REFNAME17</Cite> | |||
|- | |||
|valign="top" align="left"|Typical angina (definite) | |||
|Meets three of the following characteristics: | |||
*Substernal chest discomfort of characteristic quality and duration | |||
*Provoked by exertion or emotional stress | |||
*Relieved by rest and/or nitroglycerine | |||
|- | |||
| valign="top"|Atypical angina (probable) | |||
|Meets two of these characteristics | |||
|- | |||
| valign="top"|Non-cardiac chest pain | |||
|Meets one or none of the characteristics | |||
|} | |||
The classification of chest pain in combination with age and sex is helpful in estimating the pretest likelihood of angiographically significant coronary artery disease, see Table 2. | |||
{| class="wikitable" border="1" width="600px" | |||
|- | |||
! align="left" colspan = "7" | Table 2. Clinical pre-test probabilities <sup>a</sup> in patients with stable chest pain symptoms. <Cite>REFNAME20</Cite> | |||
== | |||
|- | |- | ||
! | | align="center"| | ||
| align="center" colspan="2" bgcolor="#FFFFFF" | <b>Typical angina</b> | |||
| align="center" colspan="2" bgcolor="#FFFFFF" | <b>Atypical angina</b> | |||
| align="center" colspan="2" bgcolor="#FFFFFF" | <b>Non-anginal pain</b> | |||
|- | |||
! Age | |||
! Men | |||
! Women | |||
! Men | |||
! Women | |||
! Men | |||
! Women | |||
|- | |||
! 30-39 | |||
| align="center" bgcolor="#F0F8FF" | 59 | |||
| align="center" bgcolor="#F0F8FF" | 28 | |||
| align="center" bgcolor="#F0F8FF" | 29 | |||
| align="center" bgcolor="#FFFFFF" | 10 | |||
| align="center" bgcolor="#F0F8FF" | 18 | |||
| align="center" bgcolor="#FFFFFF" | 5 | |||
|- | |- | ||
| | ! 40-49 | ||
| | | align="center" bgcolor="#FFCCCC" | 69 | ||
# | | align="center" bgcolor="#F0F8FF" | 37 | ||
# | | align="center" bgcolor="#F0F8FF" | 38 | ||
# | | align="center" bgcolor="#FFFFFF" | 14 | ||
# | | align="center" bgcolor="#F0F8FF" | 25 | ||
| align="center" bgcolor="#FFFFFF" | 8 | |||
|- | |- | ||
| | ! 50-59 | ||
| | | align="center" bgcolor="#FFCCCC" | 77 | ||
# | | align="center" bgcolor="#F0F8FF" | 47 | ||
# | | align="center" bgcolor="#F0F8FF" | 49 | ||
| align="center" bgcolor="#F0F8FF" | 20 | |||
| align="center" bgcolor="#F0F8FF" | 34 | |||
| align="center" bgcolor="#FFFFFF" | 12 | |||
|- | |- | ||
| | ! 60-69 | ||
| | | align="center" bgcolor="#FFCCCC" | 84 | ||
| align="center" bgcolor="#F0F8FF" | 58 | |||
| align="center" bgcolor="#F0F8FF" | 59 | |||
| align="center" bgcolor="#F0F8FF" | 28 | |||
| align="center" bgcolor="#F0F8FF" | 44 | |||
| align="center" bgcolor="#F0F8FF" | 17 | |||
|- | |- | ||
| | ! 70-79 | ||
| | | align="center" bgcolor="#FF69B4" | 89 | ||
| align="center" bgcolor="#FFCCCC" | 68 | |||
| align="center" bgcolor="#FFCCCC" | 69 | |||
| align="center" bgcolor="#F0F8FF" | 37 | |||
| align="center" bgcolor="#F0F8FF" | 54 | |||
| align="center" bgcolor="#F0F8FF" | 24 | |||
|- | |- | ||
| colspan=" | ! >80 | ||
< | | align="center" bgcolor="#FF69B4" | 93 | ||
| align="center" bgcolor="#FFCCCC" | 76 | |||
| align="center" bgcolor="#FFCCCC" | 78 | |||
| align="center" bgcolor="#F0F8FF" | 47 | |||
| align="center" bgcolor="#F0F8FF" | 65 | |||
| align="center" bgcolor="#F0F8FF" | 32 | |||
|- | |||
| colspan = "7" bgcolor="#FFFFFF"| | |||
|- | |||
! colspan = "7" | ECG = electrocardiogram; PTP = pre-test probability; SCAD = stable coronary artery disease. | |||
|- | |||
| colspan = "7" bgcolor="#FFFFFF" | <b><sup>a</sup></b> Probabilities of obstructive coronary disease shown reflect the estimates for patients aged 35, 45, 55, 65, 75 and 85 years. | |||
*Groups in <i>white boxes</i> have a PTP <15% and hence can be managed without further testing. | |||
*Groups in <i>blue boxes</i> have a PTP of 15–65%. They could have an exercise ECG if feasible as the initial test. However, if local expertise and availability permit a non-invasive imaging based test for ischaemia this would be preferable given the superior diagnostic capabilities of such tests. In young patients radiation issues should be considered. | |||
*Groups in <i>light pink boxes</i> have PTPs between 66–85% and hence should have a non-invasive imaging functional test for making a diagnosis of SCAD. | |||
*In groups in <i>dark pink boxes</i> the PTP is >85% and one can assume that SCAD is present. They need risk stratification only. | |||
|} | |} | ||
The severity of complaints can be classified according to the Canadian Cardiovascular Society as shown in Table 3 | |||
{| class="wikitable" border="1" width="600px" | |||
|- | |||
= | ! colspan="2" | Table 3. Classification of angina severity according to the Canadian Cardiovascular Society | ||
|- | |||
! width="100"| ''Class'' | |||
| ''Level of Symptoms'' | |||
|- | |||
! valign="top"| Class I | |||
| 'Ordinary activity does not cause angina' | |||
Angina with strenuous or rapid or prolonged exertion only | |||
|- | |||
! valign="top"| Class II | |||
| 'Slight limitation of ordinary activity' | |||
Angina on walking or climbing stairs rapidly, walking uphill or exertion after meals, in cold weather, when under emotional stress, or only during the first few hours after awakening | |||
|- | |||
! valign="top"| Class III | |||
| 'Marked limitation of ordinary physical activity' | |||
Angina on walking one or two blocks on the level or one flight of stairs at a normal pace under normal conditions | |||
|- | |||
! valign="top"| Class IV | |||
| 'Inability to carry out physical activity without discomfort' or 'angina at rest' | |||
|} | |||
During angina pectoris ‘vegetative’ symptoms can occur, including sweating, nausea, paleface, anxiety and agitation. This is probably caused by the autonomic nerve system in reaction to stress. <Cite>REFNAME9</Cite> | |||
Finally, it is important to differentiate unstable angina (indicating an acute coronary syndrome or even myocardial infarction requiring urgent treatment) from stable angina. Unstable angina typically is severe, occurs without typical provocation and does not disappear with rest, and has a longer duration than stable angina. It is important to initiate prompt treatment in these patients, as described in the acute coronary syndromes chapter. | |||
It is important to | |||
==Physical Examination== | ==Physical Examination== | ||
There are no specific signs in angina pectoris. Physical examination of a patient with (suspected) angina pectoris is important to assess the presence of hypertension, | |||
valvular heart disease (in particular aortic valve stenosis) or hypertrophic obstructive cardiomyopathy. It should include the body-mass index, evidence of non-coronary vascular disease which may be asymptomatic and other signs of co-morbid conditions. E.g.: absence of palpable pulsations in the dorsal foot artery is associated with an 8 fold increase in the likelihood of coronary artery disease. | |||
==Electrocardiogram (ECG)== | |||
The electrocardiogram (ECG) is an important tool to differentiate between unstable angina (acute coronary syndrome) and stable angina in addition to the patient’s history. Patients with unstable angina pectoris are likely to show abnormalities on the ECG at rest, in particular ST-segment deviations. | |||
Although a resting ECG may show signs of coronary artery disease such as pathological Q-waves indicating a previous MI or other abnormalities, many patients with stable angina pectoris have a normal ECG at rest. Therefore exercise ECG testing may be necessary to show signs of myocardial ischemia. <Cite>REFNAME10</Cite> | |||
'''Exercise ECG testing''' is performed with gradually increasing intensity on a treadmill or a bicycle ergo-meter. Exercise increases the oxygen demand of the heart, potentially revealing myocardial ischemia by the occurrence of ST-segment depression on the ECG. <Cite>REFNAME11</Cite> | |||
== | ==Laboratory Testing== | ||
Laboratory testing in the setting of angina pectoris can be useful to differentiate between different causes of the pain, including an acute coronary syndrome in which there will be elevation of the marker of myocardial necrosis. Anaemia should be ruled out as a cause of ischemia. Renal function is important for pharmacological therapy. Moreover, it might assist in establishing a cardiovascular risk profile. | |||
==Stress Testing in Combination with Imaging== | |||
Some patients are unable to perform physical exercise. Furthermore, in patients with resting ECG abnormalities the exercise ECG is associated with low sensitivity and specificity. | |||
{| class="wikitable" border="1" width="600px" | |||
|- | |||
|colspan = "7" | <b>Table 4. Characteristics of tests commonly used to diagnose the presence of coronary artery disease. <Cite>REFNAME20</Cite></b> | |||
|- | |||
| bgcolor="#FFFFFF" rowspan="2"| | |||
|align="center" colspan="2" bgcolor="#FFFFFF" | <b>Diagnosis of CAD</b> | |||
|- | |||
| align="center" bgcolor="#FFFFFF" | <b>Sensitivity (%)</b> | |||
| align="center" bgcolor="#FFFFFF" | <b>Specificity (%)</b> | |||
|- | |||
| <b>Exercise ECG <sup>a, 91, 94, 95</sup></b> | |||
!45–50 | |||
!85–90 | |||
|- | |||
| <b>Exercise stress echocardiography <sup>96</sup></b> | |||
!80–85 | |||
!80–88 | |||
|- | |||
| <b>Exercise stress SPECT <sup>96-99</sup></b> | |||
!73–92 | |||
!63–87 | |||
|- | |||
| <b>Dobutamine stress echocardiography <sup>96</sup></b> | |||
!79–83 | |||
!82–86 | |||
|- | |||
| <b>Dobutamine stress MRI <sup>b,100</sup></b> | |||
!79–88 | |||
!81–91 | |||
|- | |||
| <b>Vasodilator stress echocardiography <sup>96</sup></b> | |||
!72–79 | |||
!92–95 | |||
|- | |||
| <b>Vasodilator stress SPECT <sup>96, 99</sup></b> | |||
!90–91 | |||
!75–84 | |||
|- | |||
| <b>Vasodilator stress MRI <sup>b,98, 100-102</sup></b> | |||
!67–94 | |||
!61–85 | |||
|- | |||
| <b>Coronary CTA <sup>c,103-105</sup></b> | |||
!95–99 | |||
!64–83 | |||
|- | |||
| <b>Vasodilator stress PET <sup>97, 99, 106</sup></b> | |||
!81–97 | |||
!74–91 | |||
|- | |||
| colspan="3" bgcolor="#FFFFFF"| <b>CAD</b> = coronary artery disease; <b>CTA</b> = computed tomography angiography; <b>ECG</b> = electrocardiogram; <b>MRI</b> = magnetic resonance imaging; <b>PET</b> = positron emission tomography; <b>SPECT</b> = single photon emission computed tomography. | |||
|- | |||
| colspan="3"|<b><sup>a</sup></b> Results without/with minimal referral bias. | |||
<b><sup>b</sup></b> Results obtained in populations with medium-to-high prevalence of disease without compensation for referral bias. | |||
<b><sup>c</sup></b> Results obtained in populations with low-to-medium prevalence of disease. | |||
|} | |||
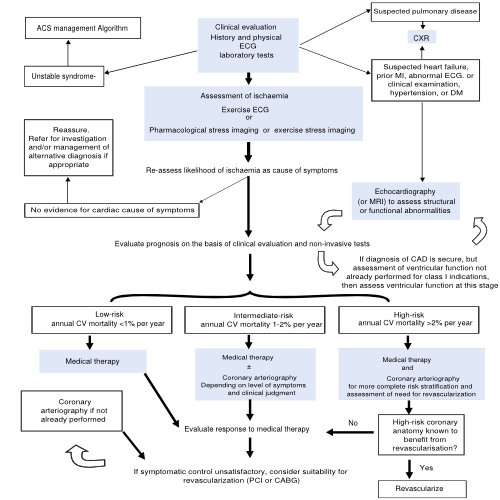
[[File:Algorithm_for_the_initial_evaluation_of_patients_with_clinical_symptoms_of_angina.svg|thumb|right|500px|Figure 1. Algorithm for the initial evaluation of patients with clinical symptoms of angina]] | |||
If the ECG made during exercise testing does not show any abnormalities myocardial ischemia becomes unlikely as cause of the complaints. If the diagnosis is still in doubt, the following additional tests may be performed. | |||
#Exercise echocardiography means that an echocardiography is made before and during different stages up to peak exercise in order to identify wall motion abnormalities. <Cite>REFNAME12</Cite> An alternative is pharmacological stress testing using dobutamine. | |||
#Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest based on radiopharmaceutical tracer uptake . <Cite>REFNAME13</Cite> | |||
#Magnetic Resonance Imaging can be done with vasodilatory adenosine or stimulating dobutamine to detect wall motion abnormalities induced by ischemia during pharmacological stress. <Cite>REFNAME14</Cite> | |||
The findings on stress testing can be used to determine the choice between medical therapy only or medical therapy and invasive assessment of the coronary anatomy in patients with stable angina. Coronary angiography is recommended based upon the severity of symptoms, likelihood of ischemic disease, and risk of the patient for subsequent complications including mortality based on risk scores. <Cite>REFNAME15</Cite> For the algorithm for the initial evaluation of patients with clinical symptoms of angina see Figure 1. | |||
==Coronoary Angiography== | |||
Coronary angiography (CAG) can assist in the diagnosis and the selection of treatment options for stable angina pectoris. During CAG, the coronary anatomy is visualized including the presence of coronary luminal stenoses. A catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. The contrast is made visible by X ray and the images that are obtained are called angiograms. | |||
If stenoses are visible, the operator will judge whether this stenosis is significant and eligible for percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). | |||
==Treatment== | |||
Stable angina pectoris is always treated with medical therapy aimed at reducing risk and at alleviating symptoms. Current guidelines recommend revascularization in patients with persistent symptoms despite optimal medical therapy. <Cite>REFNAME16</Cite> Furthermore, revascularization is indicated in case of large areas of myocardial ischemia (such as a left main stem stenosis, a proximal LAD stenosis or significant three vessel disease) and in the presence of high-risk features such as ventricular arrhythmia, heart failure, widening of QRS during ischemia, axis deviation during ischemia or hypotension during ischemia. The choice between PCI and CABG depends on the coronary anatomy and clinical characteristics and the choice should be made in a team including (interventional) cardiologists and thoracic surgeons. | |||
==Medical Therapy== | |||
Initial treatment of stable angina pectoris focuses on medication reducing the oxygen demand of the heart. ß blockers lower heart rate and blood pressure. <Cite>REFNAME17</Cite> Nitrates dilatate the coronary arteries and reduce venous return if used to abort an episode of pain. <Cite>REFNAME18</Cite> Antiplatelet therapy (aspirin) reduces the risk of development of a thrombus and thus acute (coronary) ischemic events. <Cite>REFNAME19</Cite> | |||
Risk factors like smoking, overweight, hypertension, dyslipidemia and diabetes need to be treated in order to prevent disease progression and future events. See chronic coronary diseases. | |||
== | ==PCI== | ||
The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought to the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent collapse of the arteric wall and restenosis, a stent is often positioned at the site of the stenosis. | |||
== | ==CABG== | ||
With CABG, a bypass is placed around the stenosis using the internal thoracic arteries or the saphenous veins from the legs. The bypass originates proximal from the stenosis and terminates distally from the stenosis. The operation usually requires the use of cardiopulmonary bypass and cardiac arrest, however in certain cases the grafts can be placed on the beating heart (“off-pump” surgery) | |||
== References == | |||
== | |||
<biblio> | <biblio> | ||
# | #REFNAME1 pmid=11756201 | ||
# | #REFNAME2 pmid=4997794 | ||
# | #REFNAME3 pmid=10099685 | ||
# | #REFNAME4 pmid=10866870 | ||
# | #REFNAME5 pmid=10751787 | ||
# | #REFNAME6 pmid=6831781 | ||
# | #REFNAME7 pmid=3925741 | ||
# | #REFNAME8 pmid=14678917 | ||
# | #REFNAME9 pmid=15289388 | ||
# | #REFNAME10 pmid=8375424 | ||
#REFNAME11 pmid=17162834 | |||
# | #REFNAME12 pmid=1352191 | ||
# | #REFNAME13 pmid=2007701 | ||
# | #REFNAME14 pmid=12566362 | ||
# | #REFNAME15 pmid=18061078 | ||
# | #REFNAME16 pmid=20802248 | ||
# | #REFNAME17 pmid=16735367 | ||
# | #REFNAME18 pmid=3925741 | ||
# | #REFNAME19 pmid=9355934 | ||
# | #REFNAME20 pmid=23996286 | ||
# | |||
</biblio> | </biblio> | ||
Latest revision as of 12:50, 16 September 2013
Stable angina (pectoris) is a clinical syndrome characterized by discomfort in the chest, jaw, shoulder, back, or arms, typically elicited by exertion or emotional stress and relieved by rest or nitroglycerin. It can be attributed to myocardial ischemia which is most commonly caused by atherosclerotic coronary artery disease or aortic valve stenosis.
Three major coronary arteries supply the heart with oxygenated blood, the right coronary artery (RCA), the left anterior descending coronary artery (LAD) and the left circumflex artery (LCx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries progressively narrow, a dysbalance between myocardial oxygen supply and myocardial oxygen consumption may occur, causing myocardial ischemia. In stable angina this imbalance mainly occurs when oxygen demand increases due to exercise, increased heart rate, contractility or wall stress.
A complete history and physical examination are essential to support the diagnosis (stable) angina pectoris and to exclude other (acute) causes of chest pain such as an acute coronary syndrome, aortic dissection, arrhythmias, pulmonary embolism, (tension) pneumothorax or pneumonia, gastroesophageal reflux or spams, hyperventilation or musculoskeletal pain. [1] In addition, laboratory tests and specific cardiac investigations are often necessary.
History
Patients often describe angina pectoris as pressure, tightness, or heaviness located centrally in the chest, and sometimes as strangling, constricting, or burning. The pain often radiates elsewhere in the upper body, mainly arms, jaw and/or back. [2] Some patients only complain about abdominal pain so the presentation can be aspecific. [3], [4]
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is usually is brief and gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain does not change with respiration or position. If patients had angina pectoris previously they are often able to recognize the pain immediately. [5] Angina pectoris is a manifestation of arterial insufficiency and usually occurs with increasing oxygen demand such as during exercise. As soon as the demand is decreased (by stopping the exercise for example) complaints usually disappears within a few minutes. Another way to relieve pain is by administration of nitro-glycerine. Nitro-glycerine spray is a vasodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also dilates the coronary arteries and increases coronary blood flow. [6] The response to nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine relaxes smooth muscle tissue. [7]
Depending on the characteristics, chest pain can be identified as typical angina, atypical angina or non-cardiac chest pain, see Table 1.
| Table 1. Clinical classification of chest pain [8] | |
|---|---|
| Typical angina (definite) | Meets three of the following characteristics:
|
| Atypical angina (probable) | Meets two of these characteristics |
| Non-cardiac chest pain | Meets one or none of the characteristics |
The classification of chest pain in combination with age and sex is helpful in estimating the pretest likelihood of angiographically significant coronary artery disease, see Table 2.
| Table 2. Clinical pre-test probabilities a in patients with stable chest pain symptoms. [9] | ||||||
|---|---|---|---|---|---|---|
| Typical angina | Atypical angina | Non-anginal pain | ||||
| Age | Men | Women | Men | Women | Men | Women |
| 30-39 | 59 | 28 | 29 | 10 | 18 | 5 |
| 40-49 | 69 | 37 | 38 | 14 | 25 | 8 |
| 50-59 | 77 | 47 | 49 | 20 | 34 | 12 |
| 60-69 | 84 | 58 | 59 | 28 | 44 | 17 |
| 70-79 | 89 | 68 | 69 | 37 | 54 | 24 |
| >80 | 93 | 76 | 78 | 47 | 65 | 32 |
| ECG = electrocardiogram; PTP = pre-test probability; SCAD = stable coronary artery disease. | ||||||
a Probabilities of obstructive coronary disease shown reflect the estimates for patients aged 35, 45, 55, 65, 75 and 85 years.
| ||||||
The severity of complaints can be classified according to the Canadian Cardiovascular Society as shown in Table 3
| Table 3. Classification of angina severity according to the Canadian Cardiovascular Society | |
|---|---|
| Class | Level of Symptoms |
| Class I | 'Ordinary activity does not cause angina'
Angina with strenuous or rapid or prolonged exertion only |
| Class II | 'Slight limitation of ordinary activity'
Angina on walking or climbing stairs rapidly, walking uphill or exertion after meals, in cold weather, when under emotional stress, or only during the first few hours after awakening |
| Class III | 'Marked limitation of ordinary physical activity'
Angina on walking one or two blocks on the level or one flight of stairs at a normal pace under normal conditions |
| Class IV | 'Inability to carry out physical activity without discomfort' or 'angina at rest' |
During angina pectoris ‘vegetative’ symptoms can occur, including sweating, nausea, paleface, anxiety and agitation. This is probably caused by the autonomic nerve system in reaction to stress. [10]
Finally, it is important to differentiate unstable angina (indicating an acute coronary syndrome or even myocardial infarction requiring urgent treatment) from stable angina. Unstable angina typically is severe, occurs without typical provocation and does not disappear with rest, and has a longer duration than stable angina. It is important to initiate prompt treatment in these patients, as described in the acute coronary syndromes chapter.
Physical Examination
There are no specific signs in angina pectoris. Physical examination of a patient with (suspected) angina pectoris is important to assess the presence of hypertension, valvular heart disease (in particular aortic valve stenosis) or hypertrophic obstructive cardiomyopathy. It should include the body-mass index, evidence of non-coronary vascular disease which may be asymptomatic and other signs of co-morbid conditions. E.g.: absence of palpable pulsations in the dorsal foot artery is associated with an 8 fold increase in the likelihood of coronary artery disease.
Electrocardiogram (ECG)
The electrocardiogram (ECG) is an important tool to differentiate between unstable angina (acute coronary syndrome) and stable angina in addition to the patient’s history. Patients with unstable angina pectoris are likely to show abnormalities on the ECG at rest, in particular ST-segment deviations. Although a resting ECG may show signs of coronary artery disease such as pathological Q-waves indicating a previous MI or other abnormalities, many patients with stable angina pectoris have a normal ECG at rest. Therefore exercise ECG testing may be necessary to show signs of myocardial ischemia. [11]
Exercise ECG testing is performed with gradually increasing intensity on a treadmill or a bicycle ergo-meter. Exercise increases the oxygen demand of the heart, potentially revealing myocardial ischemia by the occurrence of ST-segment depression on the ECG. [12]
Laboratory Testing
Laboratory testing in the setting of angina pectoris can be useful to differentiate between different causes of the pain, including an acute coronary syndrome in which there will be elevation of the marker of myocardial necrosis. Anaemia should be ruled out as a cause of ischemia. Renal function is important for pharmacological therapy. Moreover, it might assist in establishing a cardiovascular risk profile.
Stress Testing in Combination with Imaging
Some patients are unable to perform physical exercise. Furthermore, in patients with resting ECG abnormalities the exercise ECG is associated with low sensitivity and specificity.
| Table 4. Characteristics of tests commonly used to diagnose the presence of coronary artery disease. [9] | ||||||
| Diagnosis of CAD | ||||||
| Sensitivity (%) | Specificity (%) | |||||
| Exercise ECG a, 91, 94, 95 | 45–50 | 85–90 | ||||
|---|---|---|---|---|---|---|
| Exercise stress echocardiography 96 | 80–85 | 80–88 | ||||
| Exercise stress SPECT 96-99 | 73–92 | 63–87 | ||||
| Dobutamine stress echocardiography 96 | 79–83 | 82–86 | ||||
| Dobutamine stress MRI b,100 | 79–88 | 81–91 | ||||
| Vasodilator stress echocardiography 96 | 72–79 | 92–95 | ||||
| Vasodilator stress SPECT 96, 99 | 90–91 | 75–84 | ||||
| Vasodilator stress MRI b,98, 100-102 | 67–94 | 61–85 | ||||
| Coronary CTA c,103-105 | 95–99 | 64–83 | ||||
| Vasodilator stress PET 97, 99, 106 | 81–97 | 74–91 | ||||
| CAD = coronary artery disease; CTA = computed tomography angiography; ECG = electrocardiogram; MRI = magnetic resonance imaging; PET = positron emission tomography; SPECT = single photon emission computed tomography. | ||||||
| a Results without/with minimal referral bias.
b Results obtained in populations with medium-to-high prevalence of disease without compensation for referral bias. c Results obtained in populations with low-to-medium prevalence of disease. | ||||||
If the ECG made during exercise testing does not show any abnormalities myocardial ischemia becomes unlikely as cause of the complaints. If the diagnosis is still in doubt, the following additional tests may be performed.
- Exercise echocardiography means that an echocardiography is made before and during different stages up to peak exercise in order to identify wall motion abnormalities. [13] An alternative is pharmacological stress testing using dobutamine.
- Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest based on radiopharmaceutical tracer uptake . [14]
- Magnetic Resonance Imaging can be done with vasodilatory adenosine or stimulating dobutamine to detect wall motion abnormalities induced by ischemia during pharmacological stress. [15]
The findings on stress testing can be used to determine the choice between medical therapy only or medical therapy and invasive assessment of the coronary anatomy in patients with stable angina. Coronary angiography is recommended based upon the severity of symptoms, likelihood of ischemic disease, and risk of the patient for subsequent complications including mortality based on risk scores. [16] For the algorithm for the initial evaluation of patients with clinical symptoms of angina see Figure 1.
Coronoary Angiography
Coronary angiography (CAG) can assist in the diagnosis and the selection of treatment options for stable angina pectoris. During CAG, the coronary anatomy is visualized including the presence of coronary luminal stenoses. A catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. The contrast is made visible by X ray and the images that are obtained are called angiograms. If stenoses are visible, the operator will judge whether this stenosis is significant and eligible for percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
Treatment
Stable angina pectoris is always treated with medical therapy aimed at reducing risk and at alleviating symptoms. Current guidelines recommend revascularization in patients with persistent symptoms despite optimal medical therapy. [17] Furthermore, revascularization is indicated in case of large areas of myocardial ischemia (such as a left main stem stenosis, a proximal LAD stenosis or significant three vessel disease) and in the presence of high-risk features such as ventricular arrhythmia, heart failure, widening of QRS during ischemia, axis deviation during ischemia or hypotension during ischemia. The choice between PCI and CABG depends on the coronary anatomy and clinical characteristics and the choice should be made in a team including (interventional) cardiologists and thoracic surgeons.
Medical Therapy
Initial treatment of stable angina pectoris focuses on medication reducing the oxygen demand of the heart. ß blockers lower heart rate and blood pressure. [8] Nitrates dilatate the coronary arteries and reduce venous return if used to abort an episode of pain. [18] Antiplatelet therapy (aspirin) reduces the risk of development of a thrombus and thus acute (coronary) ischemic events. [19] Risk factors like smoking, overweight, hypertension, dyslipidemia and diabetes need to be treated in order to prevent disease progression and future events. See chronic coronary diseases.
PCI
The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought to the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent collapse of the arteric wall and restenosis, a stent is often positioned at the site of the stenosis.
CABG
With CABG, a bypass is placed around the stenosis using the internal thoracic arteries or the saphenous veins from the legs. The bypass originates proximal from the stenosis and terminates distally from the stenosis. The operation usually requires the use of cardiopulmonary bypass and cardiac arrest, however in certain cases the grafts can be placed on the beating heart (“off-pump” surgery)
References
- Sampson JJ and Cheitlin MD. Pathophysiology and differential diagnosis of cardiac pain. Prog Cardiovasc Dis. 1971 May;13(6):507-31. DOI:10.1016/s0033-0620(71)80001-4 |
- Foreman RD. Mechanisms of cardiac pain. Annu Rev Physiol. 1999;61:143-67. DOI:10.1146/annurev.physiol.61.1.143 |
- Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, and Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000 Jun 28;283(24):3223-9. DOI:10.1001/jama.283.24.3223 |
- Pope JH, Ruthazer R, Beshansky JR, Griffith JL, and Selker HP. Clinical Features of Emergency Department Patients Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J Thromb Thrombolysis. 1998 Jul;6(1):63-74. DOI:10.1023/A:1008876322599 |
- Constant J. The clinical diagnosis of nonanginal chest pain: the differentiation of angina from nonanginal chest pain by history. Clin Cardiol. 1983 Jan;6(1):11-6. DOI:10.1002/clc.4960060102 |
- Abrams J. Hemodynamic effects of nitroglycerin and long-acting nitrates. Am Heart J. 1985 Jul;110(1 Pt 2):216-24.
- Henrikson CA, Howell EE, Bush DE, Miles JS, Meininger GR, Friedlander T, Bushnell AC, and Chandra-Strobos N. Chest pain relief by nitroglycerin does not predict active coronary artery disease. Ann Intern Med. 2003 Dec 16;139(12):979-86. DOI:10.7326/0003-4819-139-12-200312160-00007 |
- Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, De Backer G, Hjemdahl P, Lopez-Sendon J, Marco J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, Priori SG, Blanc JJ, Budaj A, Camm J, Dean V, Deckers J, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo J, Zamorano JL, Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology, and ESC Committee for Practice Guidelines (CPG). Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J. 2006 Jun;27(11):1341-81. DOI:10.1093/eurheartj/ehl001 |
- Task Force Members, Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di Mario C, Ferreira JR, Gersh BJ, Gitt AK, Hulot JS, Marx N, Opie LH, Pfisterer M, Prescott E, Ruschitzka F, Sabaté M, Senior R, Taggart DP, van der Wall EE, Vrints CJ, ESC Committee for Practice Guidelines, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Document Reviewers, Knuuti J, Valgimigli M, Bueno H, Claeys MJ, Donner-Banzhoff N, Erol C, Frank H, Funck-Brentano C, Gaemperli O, Gonzalez-Juanatey JR, Hamilos M, Hasdai D, Husted S, James SK, Kervinen K, Kolh P, Kristensen SD, Lancellotti P, Maggioni AP, Piepoli MF, Pries AR, Romeo F, Rydén L, Simoons ML, Sirnes PA, Steg PG, Timmis A, Wijns W, Windecker S, Yildirir A, and Zamorano JL. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013 Oct;34(38):2949-3003. DOI:10.1093/eurheartj/eht296 |
- Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, and American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004 Aug 3;110(5):588-636. DOI:10.1161/01.CIR.0000134791.68010.FA |
- Guidelines for cardiac exercise testing. ESC Working Group on Exercise Physiology, Physiopathology and Electrocardiography. Eur Heart J. 1993 Jul;14(7):969-88.
- Fox K, García MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, de Backer G, Hjemdahl P, López-Sendón J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, and Grupo de trabajo de la sociedad europea de cardiologia sobre el manejo de la angina estable. [Guidelines on the management of stable angina pectoris. Executive summary]. Rev Esp Cardiol. 2006 Sep;59(9):919-70. DOI:10.1157/13092800 |
- Amanullah AM and Lindvall K. Predischarge exercise echocardiography in patients with unstable angina who respond to medical treatment. Clin Cardiol. 1992 Jun;15(6):417-23. DOI:10.1002/clc.4960150605 |
- Brown KA. Prognostic value of thallium-201 myocardial perfusion imaging in patients with unstable angina who respond to medical treatment. J Am Coll Cardiol. 1991 Apr;17(5):1053-7. DOI:10.1016/0735-1097(91)90829-x |
- Kwong RY, Schussheim AE, Rekhraj S, Aletras AH, Geller N, Davis J, Christian TF, Balaban RS, and Arai AE. Detecting acute coronary syndrome in the emergency department with cardiac magnetic resonance imaging. Circulation. 2003 Feb 4;107(4):531-7. DOI:10.1161/01.cir.0000047527.11221.29 |
- Fraker TD Jr, Fihn SD, 2002 Chronic Stable Angina Writing Committee, American College of Cardiology, American Heart Association, Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, Ferguson TB Jr, Gardin JM, O'Rourke RA, Williams SV, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, and Yancy CW. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol. 2007 Dec 4;50(23):2264-74. DOI:10.1016/j.jacc.2007.08.002 |
- Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS), European Association for Percutaneous Cardiovascular Interventions (EAPCI), Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, and Taggart D. Guidelines on myocardial revascularization. Eur Heart J. 2010 Oct;31(20):2501-55. DOI:10.1093/eurheartj/ehq277 |
- Abrams J. Hemodynamic effects of nitroglycerin and long-acting nitrates. Am Heart J. 1985 Jul;110(1 Pt 2):216-24.
- Hennekens CH, Dyken ML, and Fuster V. Aspirin as a therapeutic agent in cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1997 Oct 21;96(8):2751-3. DOI:10.1161/01.cir.96.8.2751 |
- Davies SW. Clinical presentation and diagnosis of coronary artery disease: stable angina. Br Med Bull. 2001;59:17-27. DOI:10.1093/bmb/59.1.17 |