Chest Pain / Angina Pectoris: Difference between revisions
No edit summary |
Secretariat (talk | contribs) No edit summary |
||
| Line 3: | Line 3: | ||
Three major coronary arteries provide the heart with oxygenated blood, the right coronary artery (RCA), the left coronary artery (LCA) and the circumflex artery (Cx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries narrows, the heart receives less oxygenated blood and becomes hypoxic, which results in angina pectoris. | Three major coronary arteries provide the heart with oxygenated blood, the right coronary artery (RCA), the left coronary artery (LCA) and the circumflex artery (Cx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries narrows, the heart receives less oxygenated blood and becomes hypoxic, which results in angina pectoris. | ||
Complete history and physical examination are essential to determine angina pectoris as diagnosis and to exclude other causes of chest pain, such as aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems. | Complete history and physical examination are essential to determine angina pectoris as diagnosis and to exclude other causes of chest pain, such as aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems.<cite>Sampson</cite> | ||
===History=== | ===History=== | ||
Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back. Some patients only complain about stomach ache so the presentation can be very a specific. | Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back.<cite>Foreman</cite> Some patients only complain about stomach ache so the presentation can be very a specific.<cite>Canto</cite> <cite>Pope</cite> | ||
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately. | Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately.<cite>Constant</cite> | ||
Angina pectoris usually occurs during exercise when the demand for oxygenated blood increases. Coronary arteries with a narrowed lumen can not meet the demand of oxygenated blood during exercise. As soon as the exercise is aborted angina pectoris decreases. This is called stable angina pectoris. | Angina pectoris usually occurs during exercise when the demand for oxygenated blood increases. Coronary arteries with a narrowed lumen can not meet the demand of oxygenated blood during exercise. As soon as the exercise is aborted angina pectoris decreases. This is called stable angina pectoris. | ||
Unstable angina pectoris means angina pectoris at rest which consists less than two months. Over time the angina pectoris develops to more often, severe and prolonged, so that symptoms are to occur at less and less effort than before. | Unstable angina pectoris means angina pectoris at rest which consists less than two months. Over time the angina pectoris develops to more often, severe and prolonged, so that symptoms are to occur at less and less effort than before.<cite>Anderson</cite> | ||
Stable angina pectoris responds to nitro-glycerine spray, unstable angina pectoris does not. | Stable angina pectoris responds to nitro-glycerine spray, unstable angina pectoris does not. | ||
Nitro-glycerine spray is a venodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also vasodilates the coronary arteries and increases coronary blood flow. | Nitro-glycerine spray is a venodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also vasodilates the coronary arteries and increases coronary blood flow.<cite>Abrams</cite> | ||
Nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine also relaxes smooth muscle. | Nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine also relaxes smooth muscle.<cite>Henrikson</cite> | ||
During angina pectoris so called vegetative symptoms can occur, this includes sweating, nausea, paleface, anxiety and agitation. The idea is that the vegetative nerve system is more active in a reaction to stress. | During angina pectoris so called vegetative symptoms can occur, this includes sweating, nausea, paleface, anxiety and agitation. The idea is that the vegetative nerve system is more active in a reaction to stress.<cite>Antman</cite> | ||
===Physical Examination=== | ===Physical Examination=== | ||
| Line 28: | Line 29: | ||
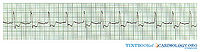
The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression. | The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression. | ||
Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities. During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities. | Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities. During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities.<cite>Fox</cite> | ||
===Additional | ===Additional Research=== | ||
If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done. Depending on the hospital one of the below standing research will be done. | If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done.<cite>Fox2</cite> Depending on the hospital one of the below standing research will be done. | ||
# Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity. | # Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity.<cite>Amanullah</cite> | ||
# Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest. | # Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest.<cite>Brown</cite> | ||
# MRI can be done with vasodilatory dobutamine or stimulating adenosine to assess how the heart behaves during exercise. | # MRI can be done with vasodilatory dobutamine or stimulating adenosine to assess how the heart behaves during exercise.<cite>Kwong</cite> | ||
The findings on stress testing can be used to determine the choice between medical therapy and revascularization in patients with stable angina. Coronary angiography is recommended based upon symptoms, left ventricular function, and estimated risk by stress testing.<cite>Fraker</cite> | |||
===Cardiac Markers=== | ===Cardiac Markers=== | ||
| Line 68: | Line 69: | ||
<biblio> | <biblio> | ||
#Davies pmid=11756201 | #Davies pmid=11756201 | ||
#Sampson pmid=4997794 | |||
#Foreman pmid=10099685 | |||
#Canto pmid=10866870 | |||
#Pope pmid=10751787 | |||
#Constant pmid=6831781 | |||
#Anderson pmid=17692738 | |||
#Abrams pmid=3925741 | |||
#Henrikson pmid=14678917 | |||
#Antman pmid=15289388 | |||
#Fox pmid=17162834 | |||
#Fox2 pmid=17162834 | |||
#Amanullah pmid=1352191 | |||
#Brown pmid=2007701 | |||
#Kwong pmid=12566362 | |||
#Fraker pmid=18061078 | |||
</biblio> | </biblio> | ||
Revision as of 03:11, 10 August 2011
In 1772 doctor William Heberden first described angina pectoris, he wrote: “They who are afflicted with it are seized, while they are walking (more especially if it be up hill), with a painful and most disagreeable sensation in the breast, which seems as if it would extinguish life if it were to increase or to continue, but the moment the patient stands still all this uneasiness vanishes”.[1]
Three major coronary arteries provide the heart with oxygenated blood, the right coronary artery (RCA), the left coronary artery (LCA) and the circumflex artery (Cx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries narrows, the heart receives less oxygenated blood and becomes hypoxic, which results in angina pectoris.
Complete history and physical examination are essential to determine angina pectoris as diagnosis and to exclude other causes of chest pain, such as aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems.[2]
History
Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back.[3] Some patients only complain about stomach ache so the presentation can be very a specific.[4] [5]
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately.[6]
Angina pectoris usually occurs during exercise when the demand for oxygenated blood increases. Coronary arteries with a narrowed lumen can not meet the demand of oxygenated blood during exercise. As soon as the exercise is aborted angina pectoris decreases. This is called stable angina pectoris. Unstable angina pectoris means angina pectoris at rest which consists less than two months. Over time the angina pectoris develops to more often, severe and prolonged, so that symptoms are to occur at less and less effort than before.[7]
Stable angina pectoris responds to nitro-glycerine spray, unstable angina pectoris does not. Nitro-glycerine spray is a venodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also vasodilates the coronary arteries and increases coronary blood flow.[8]
Nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine also relaxes smooth muscle.[9]
During angina pectoris so called vegetative symptoms can occur, this includes sweating, nausea, paleface, anxiety and agitation. The idea is that the vegetative nerve system is more active in a reaction to stress.[10]
Physical Examination
Oxygen deficiency of the heart leads to ischemia, ischemia and the discomfort the patient experiences lead to sympathetic activation of the nervous system. This is detectable during physical examination by an increase in heart rate and elevation in blood pressure. Ischemia can also cause a temporarily impairment in myocardial function, on auscultation you could hear a paradoxically split second heart sound, a third or fourth heart sound and a mitral regurgitation murmur. All these findings however disappear with resolution of the ischemia
ECG
The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression.
Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities. During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities.[11]
Additional Research
If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done.[12] Depending on the hospital one of the below standing research will be done.
- Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity.[13]
- Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest.[14]
- MRI can be done with vasodilatory dobutamine or stimulating adenosine to assess how the heart behaves during exercise.[15]
The findings on stress testing can be used to determine the choice between medical therapy and revascularization in patients with stable angina. Coronary angiography is recommended based upon symptoms, left ventricular function, and estimated risk by stress testing.[16]
Cardiac Markers
In addition to an ECG it is common to take blood samples and run the blood for elevated cardiac markers. Elevated CK MB and Troponin I indicate ischemia. It can however take 4-8 hours, after the symptoms started, before CK MB is elevated. The same applies to Troponin I, the advise is to repeat the measurements after 4-6 hours. A pitfall concerning elevated Troponin I can be patients with renal failure or pulmonary embolism. Positive cardiac markers indicate non ST elevation MI (NSTEMI), negative cardiac markers indicate unstable angina pectoris.
Treatment
Medication
In patients with stable angina pectoris with little or no symptoms and no abnormalities found during additional research, treatment focuses on preventing angina pectoris and reducing the risk of a heart attack to a minimum. Therefore medication, all aimed to keep the workload of the heart as low as possible, will be necessary. β blockers lower heart rate and blood pressure, this decreases the oxygen demand of the heart. Nitrates dilatate the coronary arteries so the heart receives more oxygenated blood. Anticoagulants reduce the risk of development of a thrombus in the coronary arteries. Statins to lower cholesterol levels.
Apart from starting medication the patient needs to minimize any present risk factors like smoking, overweight and drinking alcohol. See chronic coronary diseases.
Coronary Angiography
Coronary angiography (CAG) is an X ray examination of the coronary arteries, a catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. Contrast is visible by X ray and the images that are obtained are called angiograms. On an angiogram stenoses will be visible, if the stenosis is significant coronary intervention will take place. Ideally this happens immediately following the CAG but not all hospitals that are entitled to carry out CAG are qualified to perform percutaneous coronary intervention (PCI).
Percutaneous Coronary Intervention
The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is often positioned at the site of the stenosis.
Coronary Artery Bypass Graft
When the coronary arteries contain too many or too severe stenoses for PCI a coronary artery bypass graft (CABG) is indicated. Especially when the stenoses are located proximally of the three major coronary arteries, causing occlusion of many ramifications and high risk of severe myocardial damage.
CABG does not eliminate the stenosis like PCI does. Using the internal thoracic arteries or the saphenous veins from the legs a bypass is made around the stenosis. The bypass originates from the aorta and terminates directly after the stenosis. Thereby restoring the blood supply to the ramifications.
A bypass can be single or multiple, multiple meaning that there are several coronary arteries bypassed using the same bypass.
References
- Davies SW. Clinical presentation and diagnosis of coronary artery disease: stable angina. Br Med Bull. 2001;59:17-27. DOI:10.1093/bmb/59.1.17 |
- Sampson JJ and Cheitlin MD. Pathophysiology and differential diagnosis of cardiac pain. Prog Cardiovasc Dis. 1971 May;13(6):507-31. DOI:10.1016/s0033-0620(71)80001-4 |
- Foreman RD. Mechanisms of cardiac pain. Annu Rev Physiol. 1999;61:143-67. DOI:10.1146/annurev.physiol.61.1.143 |
- Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, and Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000 Jun 28;283(24):3223-9. DOI:10.1001/jama.283.24.3223 |
- Pope JH, Ruthazer R, Beshansky JR, Griffith JL, and Selker HP. Clinical Features of Emergency Department Patients Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J Thromb Thrombolysis. 1998 Jul;6(1):63-74. DOI:10.1023/A:1008876322599 |
- Constant J. The clinical diagnosis of nonanginal chest pain: the differentiation of angina from nonanginal chest pain by history. Clin Cardiol. 1983 Jan;6(1):11-6. DOI:10.1002/clc.4960060102 |
- Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction), American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association of Cardiovascular and Pulmonary Rehabilitation, and Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007 Aug 14;50(7):e1-e157. DOI:10.1016/j.jacc.2007.02.013 |
- Abrams J. Hemodynamic effects of nitroglycerin and long-acting nitrates. Am Heart J. 1985 Jul;110(1 Pt 2):216-24.
- Henrikson CA, Howell EE, Bush DE, Miles JS, Meininger GR, Friedlander T, Bushnell AC, and Chandra-Strobos N. Chest pain relief by nitroglycerin does not predict active coronary artery disease. Ann Intern Med. 2003 Dec 16;139(12):979-86. DOI:10.7326/0003-4819-139-12-200312160-00007 |
- Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, and American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004 Aug 3;110(5):588-636. DOI:10.1161/01.CIR.0000134791.68010.FA |
- Fox K, García MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, de Backer G, Hjemdahl P, López-Sendón J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, and Grupo de trabajo de la sociedad europea de cardiologia sobre el manejo de la angina estable. [Guidelines on the management of stable angina pectoris. Executive summary]. Rev Esp Cardiol. 2006 Sep;59(9):919-70. DOI:10.1157/13092800 |
- Fox K, García MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, de Backer G, Hjemdahl P, López-Sendón J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, and Grupo de trabajo de la sociedad europea de cardiologia sobre el manejo de la angina estable. [Guidelines on the management of stable angina pectoris. Executive summary]. Rev Esp Cardiol. 2006 Sep;59(9):919-70. DOI:10.1157/13092800 |
- Amanullah AM and Lindvall K. Predischarge exercise echocardiography in patients with unstable angina who respond to medical treatment. Clin Cardiol. 1992 Jun;15(6):417-23. DOI:10.1002/clc.4960150605 |
- Brown KA. Prognostic value of thallium-201 myocardial perfusion imaging in patients with unstable angina who respond to medical treatment. J Am Coll Cardiol. 1991 Apr;17(5):1053-7. DOI:10.1016/0735-1097(91)90829-x |
- Kwong RY, Schussheim AE, Rekhraj S, Aletras AH, Geller N, Davis J, Christian TF, Balaban RS, and Arai AE. Detecting acute coronary syndrome in the emergency department with cardiac magnetic resonance imaging. Circulation. 2003 Feb 4;107(4):531-7. DOI:10.1161/01.cir.0000047527.11221.29 |
- Fraker TD Jr, Fihn SD, 2002 Chronic Stable Angina Writing Committee, American College of Cardiology, American Heart Association, Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, Ferguson TB Jr, Gardin JM, O'Rourke RA, Williams SV, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, and Yancy CW. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol. 2007 Dec 4;50(23):2264-74. DOI:10.1016/j.jacc.2007.08.002 |